Peptide Blog
All articles and shared info are for educational purposes only.
Latest Peptide Articles
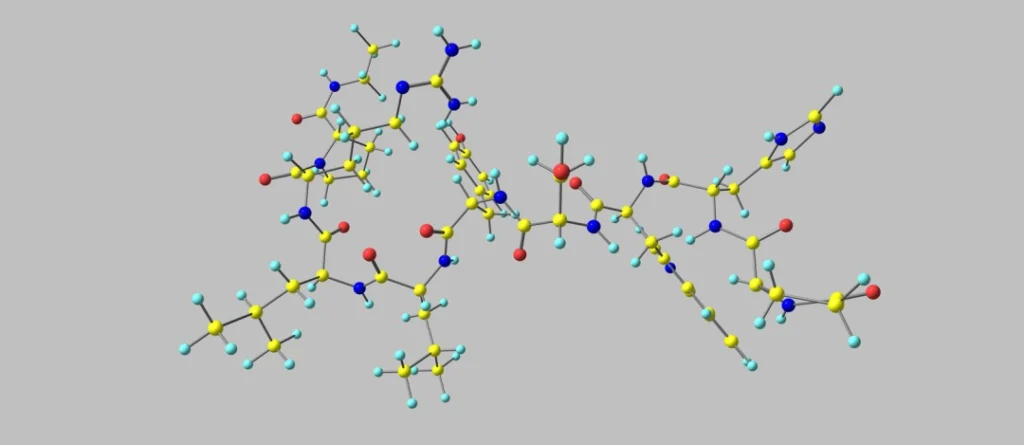
Ramatercept (ACE-031): Research Muscle Cell Homeostasis and Metabolic Integrity
ACE-031 peptide, also referred to as Ramatercept, is recognized by researchers as a recombinant protein engineered by fusing the extracellular component of activin receptor type IIB (ActRIIB) with the Fc region of IgG1. This design is suggested to support the protein’s theoretical function as a decoy receptor with high affinity for several ligands in the...
Retatrutide Peptide: Research on Metabolic Regulation and Multi-Hormonal Pathway Activation
Retatrutide is a novel investigational peptide positioned by researchers specializing in the expanding field of multi-agonist agents as an agent relevant to targeted metabolic regulation. The peptide has been classified as a GGG tri-agonist. Retatrutide has been hypothesized to display simultaneous activity at three key receptor systems implicated in energy homeostasis: the glucagon-like peptide-1 receptor...
KP-10 (Kisspeptin-10): Studies on Neuroprotection, Gonadotropin Regulation, and Emotional Processing
Kisspeptin-10 (also referred to as “KP-10”) is a short bioactive peptide fragment of the kisspeptin family, originating from proteolytic processing of a 145-amino acid precursor encoded by the KISS1 gene. This gene product is believed to undergo sequential cleavage, yielding several functional fragments, including kisspeptin-54, kisspeptin-14, kisspeptin-13, and the decapeptide Kp-10. Among these, Kp-10 corresponds...
The Synergistic Potential of Fragment 176-191 & CJC-1295 & Ipamorelin Blend in Peptide Based Studies
Recent investigations into growth hormone secretagogues (GHSs), growth hormone-releasing peptides (GHRPs), and analogs of growth hormone (hGH) have pointed to their potential in modulating endogenous hormone regulation. Individually and in combination, these agents may potentially influence physiological processes such as lipid mobilization, muscle composition, circadian rhythm modulation, and various systemic functions, including gastrointestinal and cardiovascular...
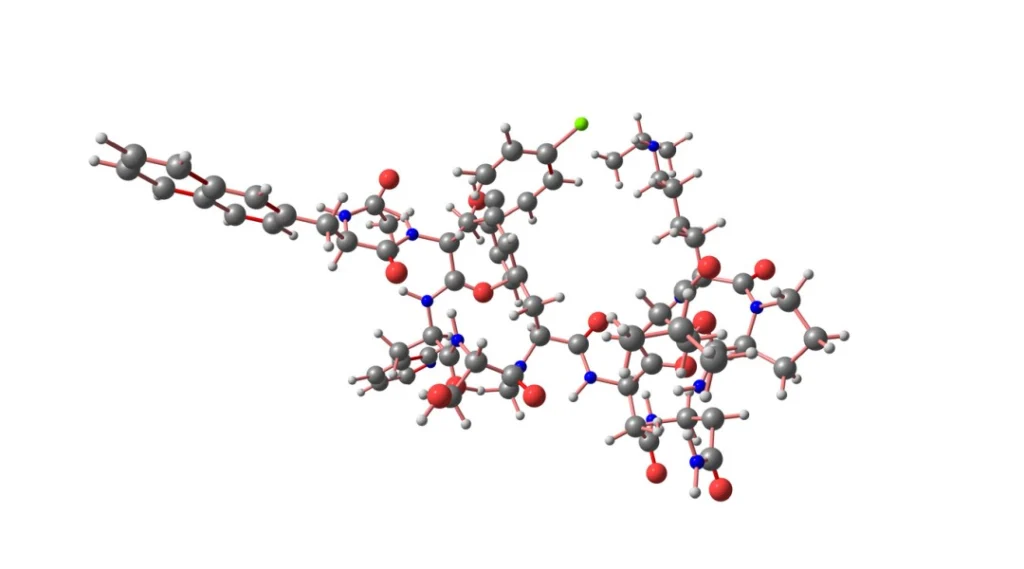
FST-344 (Follistatin-344) Peptide: Transforming Growth Factor-beta (TGF-β) Implications
Follistatin-344 (FST-344) is an endogenous glycoprotein widely distributed across various tissues. It is classified as an autocrine signaling molecule, meaning that scientists consider it to be synthesized and secreted by cells to bind to their own surface receptors, leading to intracellular modifications. Research suggests that Follistatin exists primarily in two isoforms, FST-317 and FST-344, with...
GHK-Cu and AHK-Cu: Copper Peptides and Cell Interaction Research Studies
Copper peptides are endogenously occurring complexes formed by binding copper ions (Cu2+) to specific amino acid sequences. Among these, glycyl-L-histidyl-L-lysine (GHK-Cu) is the most extensively studied tripeptide. However, other copper-binding peptides such as DAHK-Cu (Aspartyl-Alanyl-Histidyl-Lysine) and AHK-Cu (Alanine-Histidine-Lysine) have also been identified. These peptides have reportedly been studied for their potential roles in gene expression,...
Proxofim Peptide and Cellular Apoptosis: A Research Summary
FOXO4-D-Retro-Inverso (FOXO4-DRI), also called Proxofim peptide, is a synthetic variant of the endogenous FOXO4 protein. This synthetic variant is developed with D-amino acids in place of the endogenously occurring L-amino acids. This modification was made in the hope of supporting stability by reducing susceptibility to proteolytic degradation, thereby increasing the potential to extend a cellular...
Bremelanotide Peptide and HSDD Related-Research
Bremelanotide, also known as PT-141, is a synthetic cyclic heptapeptide derived from Melanotan II (MT-II), a synthetic analog of the melanocortin hormone α-melanocyte-stimulating hormone (α-MSH). It was initially investigated for its potential role in addressing hypoactive sexual desire disorder (HSDD) in female research models, as evaluated in Phase IIb clinical trials by qualified researchers. Research...
Pralmorelin Peptide and Growth Hormone Secretegogue Receptors (GHS-Rs)
Pralmorelin, also referred to as Growth Hormone Releasing Peptide-2 (GHRP-2), is a synthetic pentapeptide classified as a growth hormone secretagogue. Structurally analogous to met-enkephalin, it appears to lack opioid activity and instead interacts with the ghrelin/growth hormone secretagogue receptors (GHS-Rs) to stimulate growth hormone (GH) release. Initially developed as a diagnostic agent for assessing GH...