ARA-290 is a peptide derivative from Erythropoietin (EPO). Erythropoietin, assumed to be the primary hormone responsible for erythropoiesis, may be involved in various physiological processes, including angiogenesis, cell survival, blood pressure regulation, and potential neuroprotection in diabetic neuropathy.
<a href=”https://biotechpeptides.com/product/ara-290-16mg/” title=”Buy ARA-290 – 16mg”><strong>ARA-290</strong></a> peptide is of interest to researchers due to its speculated selective range of effects on nociception and neuroprotection, while purportedly avoiding hemopoietic actions. Researchers may suggest that these properties may play a role in wound repair in diabetes and immune modulation in autoimmune diseases.
<h2>Research Implications of ARA-290 Peptide:</h2>
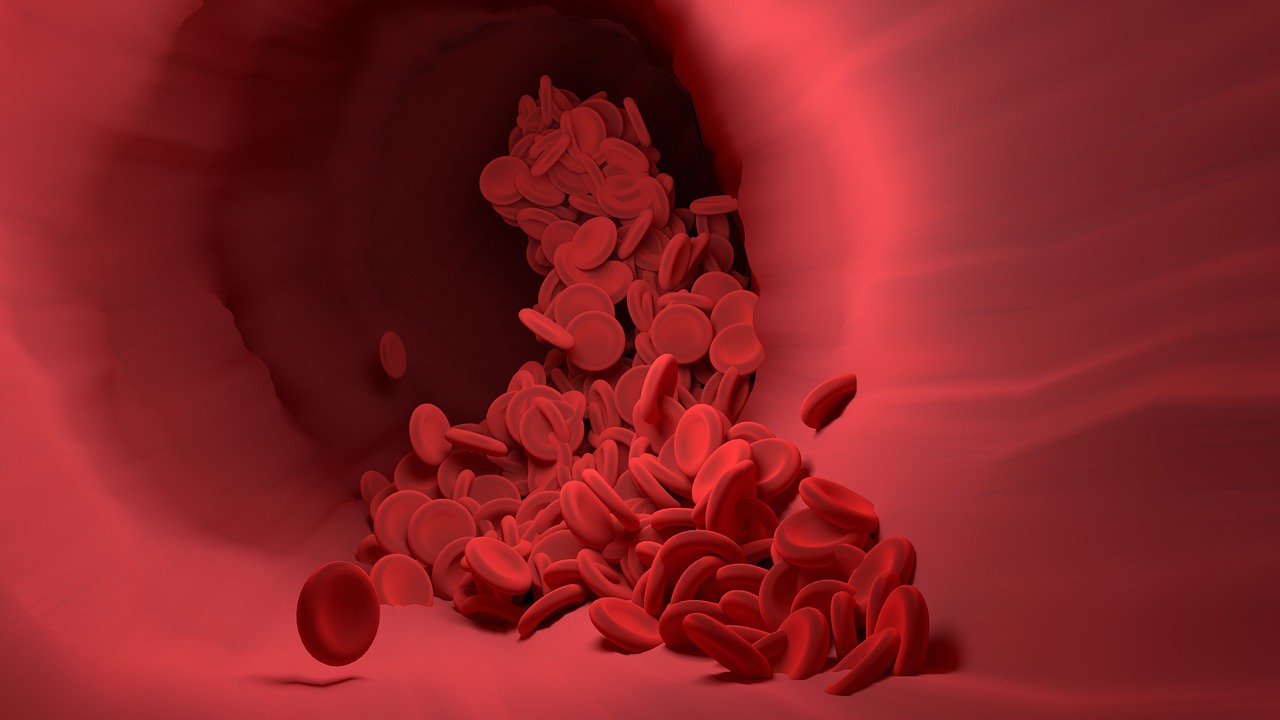
<strong>1. Blood Vessel Integrity</strong> ARA-290 peptide may play a significant role, researchers suggest, in prolonging cell survival and aiding Endothelial Colony Forming Cells (ECFCs) to repair and rebuild blood vessels after their integrity may be compromised following an injury. Similarly, researchers propose that ARA-290 peptide might protect retinal epithelial cells from ischemic or inflammatory injury, potentially promoting repair and leading to regeneration. ARA-290 is speculated to improve the migration, proliferation, and homing ability of Endothelial Colony Forming Cells, favoring the targeted repair of damaged blood vessels. Studies suggest that the peptide augments the effect of endogenous ECFCs and the transplanted exogenous ECFCs to repair and establish the vasculature of ischemic tissues.
<strong>2. Downregulation of Inflammatory Cytokines and Tissue Protection</strong> Researchers suggest that ARA-290 has the potential to suppress the inflammatory cascade by inhibiting the release of TNF-alpha, IL-6, and IL-12, speculated to prolong the survival of exogenous islet cells in diabetes. The mechanism behind this inflammatory suppression may involve the binding of the ARA-290 peptide to the Tissue Protective Receptor (TPR), reducing the effect of harmful inflammatory mediators and potentially boosting tissue protection. While erythropoietin may play a similar role, ARA-290 peptide is speculated to offer better wound healing and quicker post-injury recovery without the hematopoietic and cardiovascular effects associated with erythropoietin.
<strong>3. Role of ARA-290 in Immune System Regulation</strong> There is mounting data to suggest a role of ARA-290 peptide in immune modulation, through the binding of ARA-290 to Tissue Protective Receptors, expressed by various immune cells. After binding, ARA-290 may be expected to suppress the release of proinflammatory mediators, reducing disease severity and preventing long-term morbidity due to chronic inflammation. It may also decrease the release of inflammatory chemokines by macrophages, potentially reducing inflammatory infiltration while favoring resident macrophage recruitment to the site of injury, preventing side effects of inflammation on surrounding tissues. Studies suggest the ARA-290 peptide may alter the antigenic property of dendritic cells, potentially leading to increased long-term resistance against pathogens. This may form the foundation of its role in preventing tissue, organ, or graft rejection following transplantation. Research suggest that ARA-290 peptide has an effect on reducing levels of ANA and anti-dsDNA in Systemic Lupus Erythematous (SLE), considered markers of disease progression.
<strong>4. Nociception</strong> Researchers suggest that neuropathic pain caused by diabetic neuropathy, which is difficult to control and poorly understood, might be alleviated by suppressing Innate Repair Receptors (IRR), on which ARA-290 peptide may act. This action may inhibit TRPV1 channel (Capsaicin receptor) activity, responsible for the perception of burning pain associated with neuropathy. Studies have suggested that ARA-290 peptide exposure may increase small nerve fiber density, significantly controlling pain associated with neuropathy in several autoimmune diseases, such as sarcoidosis, diabetes, and HIV.
<em><strong>Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.</strong></em>