Thymosin Beta-4 Peptide Fragments: Anti-Inflammatory, Anti-Fibrotic, and Regenerative Properties Explored
Contents:
- Mechanisms of Action
- Scientific and Research Studies
- Thymosin Beta-4 Fragments: Functional Differentiation in Cellular Protection, Immune Modulation, and Regeneration
- Thymosin Beta-4 Fragment (1–15): Anti-Apoptotic and Neuroprotective Properties
- Thymosin Beta-4 Fragment (1–4): Anti-Inflammatory and Anti-Fibrotic Activity
- Thymosin Beta-4 Fragment (17–23): Wound Repair and Hair Follicle Regeneration
- Thymosin Beta-4 Fragment (40–43): Putative Roles in Cytoskeletal and ECM Stability
- Choosing the Right Thymosin Beta-4 Fragment
- References
Mechanism of Action
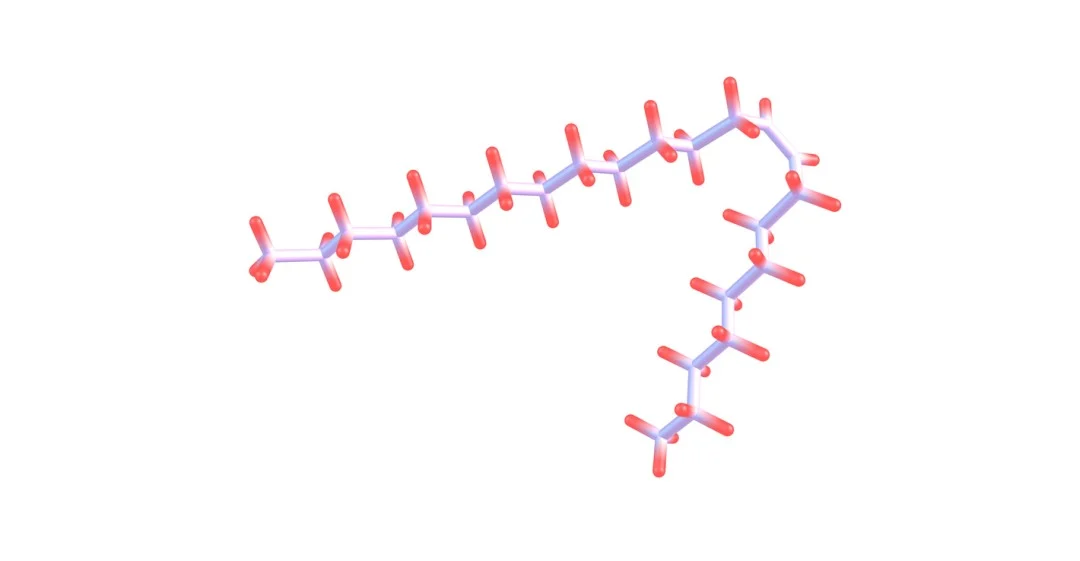
Research suggests that the full-length 43-amino acid Tβ4 peptide may undergo enzymatic cleavage, generating shorter peptide fragments with distinct and sometimes more targeted biological activities. These fragments, such as Tβ4(1–4), Tβ4(1–15), and N-acetyl-seryl-aspartyl-lysyl-proline (Ac-SDKP), retain partial sequence homology to the parent peptide but exhibit unique bioactivity profiles.
While the full-length form is generally implicated in cytoskeletal regulation and cell survival, emerging studies suggest that these particular derivatives may support specialized signaling cascades, including those involved in angiogenesis, immune response modulation, and extracellular matrix remodeling. Differentiating these fragments at the structural and functional level is critical for understanding the breadth of Tβ4’s biological roles. Ongoing peptide research conducted using murine models aims to elucidate the distinct actions of these bioactive sequences, thereby identifying their potential roles and defining their molecular mechanisms.
Scientific Research and Studies
Thymosin Beta-4 Fragments: Functional Differentiation in Cellular Protection, Immune Modulation, and Regeneration
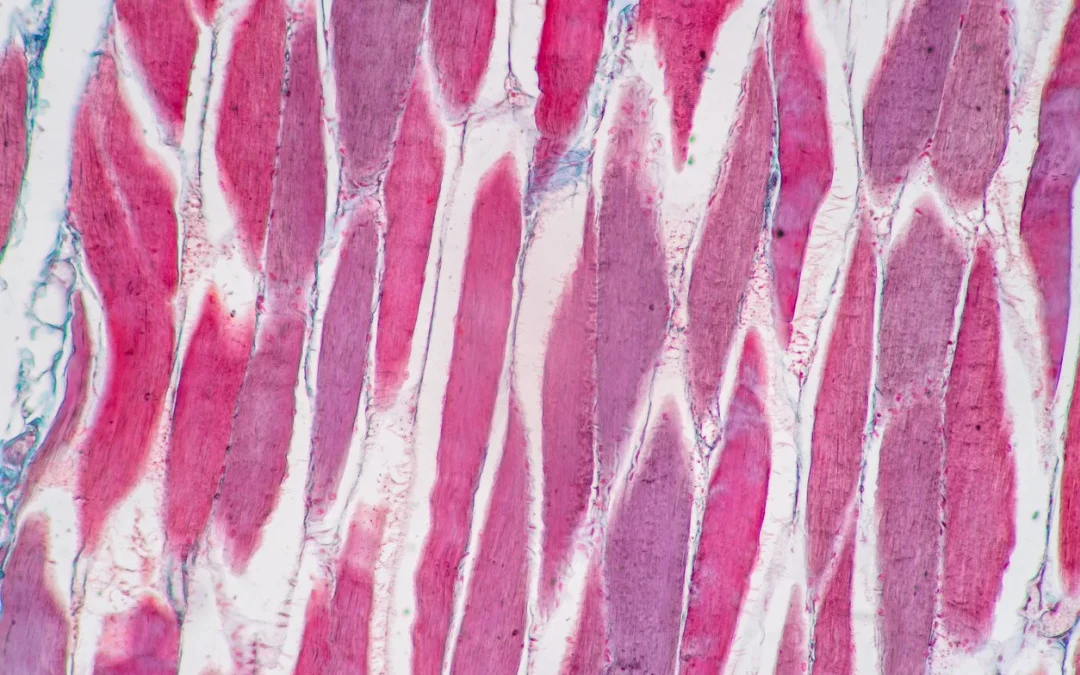
Research suggests that the full-length Thymosin Beta-4 (Tβ4) peptide is comprised of 43 amino acids. Studies have shown that the peptide exhibits a broad spectrum of biological activity across multiple tissue types. This highly conserved peptide is endogenously expressed in various cell types and is strongly associated with the regulation of cytoskeletal structures, cellular migration, and tissue remodeling processes. A central functional feature of Tβ4 is its capacity to bind monomeric G-actin. This contributes to the modulation of actin polymerization dynamics that are believed to be critical to cell motility and shape regulation.
Tβ4 has been extensively studied in experimental models of tissue injury. IN many of these studies, the peptide appears to support re-epithelialization and reduce fibrotic responses during wound repair. Researchers attribute this in part to its support of cell migration pathways and matrix remodeling. In parallel, research has suggested that Tβ4 may contribute to downregulation of pro-inflammatory mediators, such as TNF-α, IL-1β, and IL-6. This is believed to occur in tandem with the process of modulation of nuclear factor-κB (NF-κB) signaling, indicating a potential immunoregulatory role in inflammatory microenvironments.¹⁻³
Another significant function attributed to Tβ4 is its involvement in angiogenic processes. Experimental findings suggest that Tβ4 supports endothelial cell proliferation and tubule formation, implying a supportive role in neovascularization during tissue regeneration. These angiogenic supports are believed to facilitate the delivery of oxygen and nutrients to healing tissues, thereby optimizing repair kinetics.[4]
In central nervous systems observed in murine models in laboratory settings, Tβ4 has been suggested to provide potential neuroprotective support. Several studies have indicated an overall reduction in apoptotic signaling in neurons subjected to oxidative or ischemic stress. This neuroprotective activity may be mediated by the modulation of apoptotic regulators, such as Bcl-2 and caspases, although the precise intracellular pathways involved remain under investigation.⁵⁻⁶
In murine models of traumatic brain injury and stroke, Tβ4 administration has been associated with decreased lesion volume and improved functional outcomes, suggesting its relevance in neurorestorative implications.⁵ In addition to its support of neuronal and epithelial tissues, Tβ4 has been linked to dermal repair and hair follicle cycling. It has been observed to stimulate hair follicle stem cell activation and re-entry into the anagen phase in preclinical dermatologic studies, raising interest in its potential implications in hair regeneration studies conducted with murine models.⁶
While the full-length peptide orchestrates a wide array of repair and protective functions, its bioactivity is further refined through the generation of specific N- and C-terminal fragments. These include Tβ4 (1–15), Tβ4 (1–4), and Tβ4 (17–23), each suggesting specialized biological profiles. Such fragments may act independently or synergistically to regulate apoptosis, inflammation, or extracellular matrix remodeling, thereby offering a modular framework for targeted peptide research.
Thymosin Beta-4 Fragment (1–15): Anti-Apoptotic and Neuroprotective Properties
The N-terminal fragment of Thymosin Beta-4 (Tβ4), comprising the first 15 amino acids, retains essential domains involved in cytoprotection, apoptotic regulation, and cellular resilience. Tβ4 (1–15) has been identified as a bioactive region responsible for mediating cell survival signaling in multiple experimental models. Unlike the full-length peptide, this truncated form lacks actin-binding domains, yet appears to selectively regulate apoptotic and inflammatory processes through mitochondrial and transcriptional pathways.
Tβ4 (1–15) has been observed to modulate components of the intrinsic apoptotic cascade. Studies suggest that this fragment may suppress pro-apoptotic mediators, such as Bax, while upregulating anti-apoptotic proteins, including Bcl-2, thereby stabilizing mitochondrial membranes and reducing cytochrome c release. This action leads to downstream mitigation of caspase-3 activation, a key executioner in apoptosis, and may mitigate DNA fragmentation and cellular dismantling under oxidative or hypoxic stress conditions.
In neurological research conducted on mammalian research models, Tβ4 (1–15) has shown promise in models of traumatic brain injury and cerebral ischemia. The administration of the parent peptide, along with inferred fragment-specific activity, has been associated with reduced lesion volume, improved neuronal viability, and diminished neuroinflammation, which supports that it is potentially mediated by the mitigation of nuclear factor-κB (NF-κB) signaling and glial activation.[4][5] These properties suggest that Tβ4 (1–15) may contribute to both acute neuroprotection and long-term neurorestoration.
Additional studies in renal and ocular ischemia-reperfusion models have suggested the fragment’s potential to preserve tissue structure and delay the progression of apoptosis. Thymosin Beta-4 Fragment (1–15) appears to support cellular antioxidant capacity, possibly through modulation of transcriptional regulators such as FoxO3a and Nrf2.⁴ This results in improved mitochondrial integrity, decreased reactive oxygen species (ROS) accumulation, and greater resistance to metabolic stress.
Importantly, Thymosin Beta-4 Fragment (1–15) has also been implicated in regulating cellular senescence. Preclinical data suggests it may maintain redox balance by supporting NAD+/SIRT1 signaling and attenuating p53-mediated cell cycle arrest.⁵ By modulating cellular age-related signaling pathways, this fragment may delay replicative senescence and promote survival in high-turnover or stress-exposed tissues such as neurons, renal epithelial cells, and corneal endothelium.
These cumulative findings suggest that Thymosin Beta-4 Fragment (1–15) operates as a selective cytoprotective agent, acting on mitochondria-centered apoptotic pathways and inflammation-related transcriptional axes, making it a potential candidate in research addressing neurodegenerative diseases, renal injury, ischemic insult, and cellular age-associated tissue decline.
Thymosin Beta-4 Fragment (1–4): Anti-Inflammatory and Anti-Fibrotic Activity
Thymosin Beta-4 (Tβ4) Fragment (1–4), composed of the N-terminal tetra peptide N-acetyl-seryl-aspartyl-lysyl-proline (Ac-SDKP), has emerged as a bioactive molecule with pronounced anti-inflammatory and anti-fibrotic properties. Although this fragment lacks the actin-binding and cell-migratory domains of the full-length peptide, it is speculated to have a strong capacity to modulate key immune and fibrotic pathways. Due to its small size and targeted activity, Tβ4 (1–4) is widely studied in conditions driven by excessive cytokine activity, chronic inflammation, and pathological tissue remodeling.
Mechanistically, Thymosin Beta-4 Fragment (1–4) appears to exert its biological support by mitigating the activation of two principal signaling pathways involved in chronic inflammation and fibrosis: the nuclear factor-κB (NF-κB) and transforming growth factor-β1 (TGF-β1) pathways.[4] NF-κB is a transcription factor complex that orchestrates the expression of numerous pro-inflammatory cytokines, chemokines, and adhesion molecules. At the same time, TGF-β1 plays a central role in the activation of fibroblasts and the deposition of extracellular matrix (ECM) proteins, including collagen and fibronectin.
In experimental models of autoimmune and fibrotic disease, including liver fibrosis, pulmonary fibrosis, and post-infarction cardiac remodeling, administration of Thymosin Beta-4 Fragment (1–4) has been associated with a marked reduction in TNF-α, IL-1β, and IL-6 levels.[7] In parallel, the fragment suppresses ECM accumulation by downregulating collagen type I and fibronectin gene expression, thereby limiting fibrotic scarring and preserving tissue architecture. These findings suggest that Thymosin Beta-4 Fragment (1–4) functions predominantly as an immunomodulatory and fibrosis-regulatory agent, in contrast to the regenerative or anti-apoptotic focus of other Thymosin Beta-4 Fragments. Importantly, the fragment’s supports appear tissue-independent, as similar responses have been observed across hepatic, pulmonary, renal, and cardiac tissues.[5]
Unlike the full-length 43-amino acid peptide, which supports wound healing through cell migration and angiogenesis, or the 1–15 fragment that promotes survival and neuroprotection, Thymosin Beta-4 Fragment (1–4) is uniquely oriented toward controlling immune dysregulation and mitigating pathological tissue stiffening. Its role in limiting fibroblast activation, suppressing myofibroblast transformation, and maintaining ECM homeostasis positions it as a promising candidate in research on autoimmune diseases, systemic inflammatory syndromes, and organ fibrosis. These theoretical supports make Thymosin Beta-4 Fragment (1–4) particularly relevant in the context of chronic liver disease, idiopathic pulmonary fibrosis, cardiac fibrosis, and potentially neuroinflammatory conditions.
Thymosin Beta-4 Fragment (17–23): Wound Repair and Hair Follicle Regeneration
Thymosin Beta-4 (Tβ4) Fragment (17–23), also referred to by its amino acid sequence LKKTETQ, represents the actin-binding domain of the full-length peptide and plays a key role in cellular migration, cytoskeletal organization, and tissue repair. This heptapeptide fragment has been specifically associated with accelerated wound healing, angiogenesis, and hair follicle activation, distinguishing it from other Tβ4 derivatives with broader systemic support.
Mechanistically, Tβ4 (17–23) appears to support actin polymerization, a critical step in facilitating directed cell movement during injury response. By regulating cytoskeletal architecture, the fragment facilitates the migration of keratinocytes and fibroblasts, two cell types crucial for re-epithelialization and dermal repair.[7] In addition to promoting cell migration, this fragment is also said to contribute to the early inflammatory phase of wound healing by supporting mast cell degranulation. Mast cells release histamine and other mediators that recruit immune and endothelial cells to the wound site, thus initiating tissue remodeling and vascular response.²
Thymosin Beta-4 Fragment (17–23) is also linked to angiogenesis, likely through indirect stimulation of vascular endothelial cells. Improved microvascular perfusion supports oxygen and nutrient delivery to the regenerating tissue, further supporting repair processes in ischemic or injured environments. Beyond wound healing, this fragment appears to indicate activity in hair follicle regeneration. Studies suggest that it may activate quiescent follicles, prompting them to enter the anagen (growth) phase of the hair cycle.³ This support has generated interest in its potential relevance to androgenetic alopecia and cellular age-related hair thinning, particularly in exogenous or localized implications.
In contrast to other Thymosin Beta-4 Fragments, such as (1–15), which have anti-apoptotic functions, or (1–4), which exhibit anti-inflammatory supports, the 17–23 fragment is reportedly unique in targeting actin remodeling and tissue-specific regeneration, particularly within dermatological and vascular contexts.
Thymosin Beta-4 Fragment (40–43): Putative Roles in Cytoskeletal and ECM Stability
The Thymosin Beta-4 (Tβ4) Fragment (40–43) represents the C-terminal tetra-peptide of the full-length 43-amino acid sequence. While it remains the least-characterized among the major Tβ4 derivatives, emerging hypotheses have proposed possible structural and regulatory functions within cytoskeletal and extracellular matrix (ECM) environments.
Located at the terminal region of Tβ4, this sequence is unlikely to participate directly in actin sequestration like the LKKTETQ motif (residues 17–23), but its conserved positioning suggests a role in stabilizing the actin-peptide complex. It may assist in fine-tuning actin monomer binding affinity or in maintaining peptide conformational integrity, which is essential for broader cytoskeletal modulation.[2]
Additionally, Tβ4 (40–43) has been speculated to contribute to ECM interaction, potentially supporting integrin signaling or binding to fibronectin. These processes are fundamental to cell adhesion, migration, and tissue remodeling, particularly in response to injury or mechanical stress.[7]
While current data do not confirm any standalone bioactivity for this fragment, it may serve a supportive or synergistic role within the full-length peptide structure. This may involve modulating the spatial orientation of adjacent residues or facilitating the recruitment of cytoskeletal and ECM proteins during repair processes.
Given its structural location and biochemical potential, Tβ4 (40–43) remains a fragment of interest for future mechanistic studies, particularly in contexts involving tissue stability, cell-matrix interactions, and regenerative microenvironments.
Choosing the Right Thymosin Beta-4 Fragment
Thymosin Beta-4 (Tβ4) and its derived peptide fragments appear to exhibit distinct functional profiles, each associated with specific cellular and tissue-level responses. The full-length 43-amino acid peptide suggests broad relevance in regenerative implications, supporting wound repair, angiogenesis, neuroprotection, and epithelial cell survival. In contrast, its cleavage products potentially indicate specialized biological roles:
- Tβ4 (1–15) may preferentially exert anti-apoptotic and cytoprotective supports, potentially supporting neuronal and renal cell integrity under oxidative stress.
- Tβ4 (1–4) is characterized by its immunomodulatory and anti-fibrotic activity, largely mediated through suppression of inflammatory and fibrogenic cytokines.
- Tβ4 (17–23) is implicated in actin remodeling and early wound healing, with additional potential in hair follicle activation and angiogenesis.
- Tβ4 (40–43) remains the least defined, though it is hypothesized to participate in actin regulation and ECM stability.
The apparent specificity of these fragments suggests that proteolytic cleavage of Tβ4 may represent a biologically significant mechanism for localized, context-driven signaling. Selecting the appropriate Tβ4-derived sequence for experimental implications should be informed by the fragment’s predominant molecular targets, ranging from inflammatory mediators to structural proteins and mitochondrial regulators. As research progresses, fragment-specific interventions may support the precision of peptide-based approaches in inflammation, fibrosis, regeneration, and cellular aging-related degeneration.
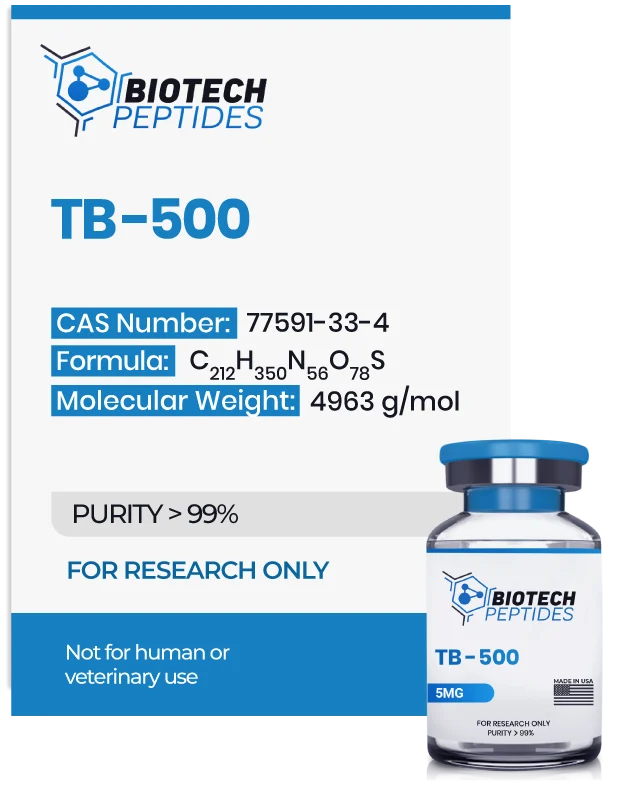
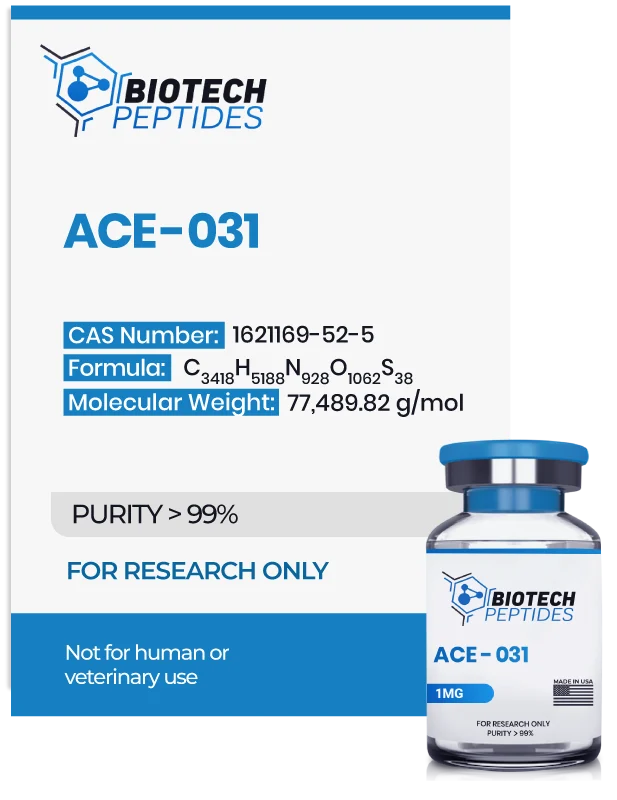
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References:
- B. Xue, R.C. Robinson, Chapter Three – Actin-Induced Structure in the Beta-Thymosin Family of Intrinsically Disordered Proteins, Editor(s): Gerald Litwack, Vitamins and Hormones, Academic Press, Volume 102, 2016, Pages 55-71, ISSN 0083-6729, ISBN 9780128048184, https://doi.org/10.1016/bs.vh.2016.04.007; https://www.sciencedirect.com/science/article/pii/S0083672916300206
- Xing Y, Ye Y, Zuo H, Li Y. Progress on the Function and Application of Thymosin β4. Front Endocrinol (Lausanne). 2021 Dec 21;12:767785. doi: 10.3389/fendo.2021.767785. PMID: 34992578; PMCID: PMC8724243. https://pmc.ncbi.nlm.nih.gov/articles/PMC8724243/
- Wang M, Feng LR, Li ZL, et al. Thymosin β4 reverses phenotypic polarization of glial cells and cognitive impairment via negative regulation of NF-κB signaling axis in APP/PS1 mice. J Neuroinflammation. 2021;18(1):146. doi:10.1186/s12974-021-02166-3. https://pubmed.ncbi.nlm.nih.gov/34183019/
- Pardon MC. Anti-inflammatory potential of thymosin β4 in the central nervous system: implications for progressive neurodegenerative diseases. Expert Opin Biol Ther. 2018;18(sup1):165-169. doi:10.1080/14712598.2018.1486817. https://pubmed.ncbi.nlm.nih.gov/30063850/
- Xiong Y, Mahmood A, Meng Y, Zhang Y, Zhang ZG, Morris DC, Chopp M. Treatment of traumatic brain injury with thymosin β4 in rats. J Neurosurg. 2011;114(1):102-115. doi:10.3171/2010.4.JNS10118. https://pmc.ncbi.nlm.nih.gov/articles/PMC3392183/
- Morris DC, Chopp M, Zhang L, Zhang ZG. Thymosin beta4: a candidate for treatment of stroke? Ann N Y Acad Sci. 2010;1194:112-117. doi:10.1111/j.1749-6632.2010.05469. https://pubmed.ncbi.nlm.nih.gov/20627173/
- Zhang G, Murthy KD, Binti Pare R, Qian Y. Protective effect of Tβ4 on central nervous system tissues and its developmental prospects. Eur J Inflammation. 2020;18. https://journals.sagepub.com/doi/10.1177/2058739220934559
- Philp D, Goldstein AL, Kleinman HK. Thymosin beta4 promotes angiogenesis, wound healing, and hair follicle development. Mech Ageing Dev. 2004 Feb;125(2):113-5. doi: 10.1016/j.mad.2003.11.005. PMID: 15037013. https://pubmed.ncbi.nlm.nih.gov/15037013/