This peptide appears to be naturally produced in the hypothalamus, where it is also known as gonadotropin-releasing hormone (GnRG), and may be rapidly degraded by enzymes called proteases. Gonadorelin appears to be a ligand for the receptors called gonadotropin-releasing hormone receptors (GnRH receptors), located on the surface of cells in the anterior pituitary gland.[1] These receptors are members of the G protein-coupled receptor (GPCR) family, which scientists characterize by their seven-transmembrane domain structure.
Activation of GnRH receptors appears to trigger intracellular signaling pathways, including the cyclic adenosine monophosphate (cAMP) pathway and the phospholipase C (PLC) pathway. These signaling pathways appear to be major regulators of the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary gland. Research indicates that these hormones may be pivotally involved in the maturation and release of eggs in the ovaries and testosterone production.
Gonadorelin (GnRH) and Gonadotropins
Gonadorelin exhibits apparent potential to bind to GnRH receptors located on pituitary cells, which may trigger a signaling cascade resulting in the transcription modulation of genes within the target cell. GnRH receptors are Gq-protein coupled, and their activation may induce the formation of receptor clusters that become internalized into the cell. Researchers should note that the GnRH receptors’ relatively short intracellular carboxy-terminal tail may prevent rapid desensitization.[2]
According to research, two potential modes of Gonadorelin action on gonadotropins are pulsatile and surge modes.[3] Pulsatile mode refers to periodic action, with clear pulses of gonadorelin into the portal circulation, while it remains undetectable between pulses. In female species, the surge mode of gonadorelin appears to occur during the preovulatory phase, where it may continuously present in the portal circulation.
Furthermore, researchers suggest that Gonadorelin may have different stimulatory actions on LH and FSH secretion, with FSH secretion being more irregular due to differences in storage, response times, and other factors. Pulsatile secretion of LH appears to be more strongly associated with Gonadorelin, while FSH has a constitutive secretion. The frequency of Gonadorelin pulses may selectively regulate gene transcription, with rapid pulses promoting LH formation and slow pulses promoting FSH formation.[4]
Moreover, scientists hypothesize that after apparent initial stimulation of FSH and LH, continuous exposure to Gonadorelin either downregulates its receptors or its signaling pathway in pituitary cells.[5] This hypothesis is based on observations that when the receptors appear to be exposed to a continuous action by gonadorelin, the “GnRH agonist (…) can actually act as an inhibitory agonist, thus reducing gonadotropin secretion.”
Gonadorelin (GnRH) and The Estrous Cycle
Scientists suggest two potential models of Gonadorelin’s action on the estrous cycle: the deterministic and permissive models. The deterministic model suggests that increasing Gonadorelin secretion may induce ovulation. In contrast, the permissive model suggests that the preovulatory LH surge may result from increased pituitary sensitivity to Gonadorelin without necessarily an increase in gonadorelin secretion. Studies in rodents, rabbits, and sheep support the deterministic model, while studies in primates suggest the permissive model may be correct.[6]
Regardless, research experiments across various animal models point to Gonadorelin’s likely role in the estrous cycle. One animal study aimed to evaluate its potential to induce ovulation in female cats.[7] The study divided 27 female cats into a Gonadorelin group and a placebo group that received saline solution. Results suggested that 84% of the female cats which received Gonadorelin had ovulated, while only 37% of the placebo group had ovulated.
One trial also aimed to assess the action of Gonadorelin on premature ovarian failure (POF) compared to a placebo for four weeks. The scientists posited that apparently, 20% of the agonist group ovulated, compared to none in the placebo group.[8] They also commented that “Follicular growth was seen in five [..] of the agonist group and in four [..] of the placebo group.” Premature ovarian failure is a condition in which the ovaries stop functioning too early. This may result in infertility, amenorrhea, dyspareunia, hyperhidrosis, etc. The cause of premature ovarian failure is not always known, but genetic factors, autoimmune disorders, and certain infections may induce it.
Gonadorelin (GnRH) and The Nervous System
Research indicates that Gonadorelin and GnRH receptors are present in different brain areas and may induce various actions. Studies hypothesize that Gonadorelin may increase the expression of cytoskeletal proteins and promote neuronal outgrowth in the cerebral cortex since GnRH receptors appear abundant amongst the neurons in these areas of the brain.[9]
Gonadorelin may also alter neural circuitry underlying visual working memory, but the mechanism of action is unclear. In the cerebellum, Gonadorelin and GnRH receptors have been reportedly detected in Purkinje cells and are suggested to potentially affect both glutamate and GABA content. In turn, this suggests a potential role in regulating their interactions.
Finally, high densities of GnRH receptors have been detected in the CA1-CA3 regions of the hippocampus, and activation of these receptors has been proposed to affect sexual behavior regulation in mammals, as well as an increase in intrinsic neuronal excitability and synaptic transmission.
Conclusion
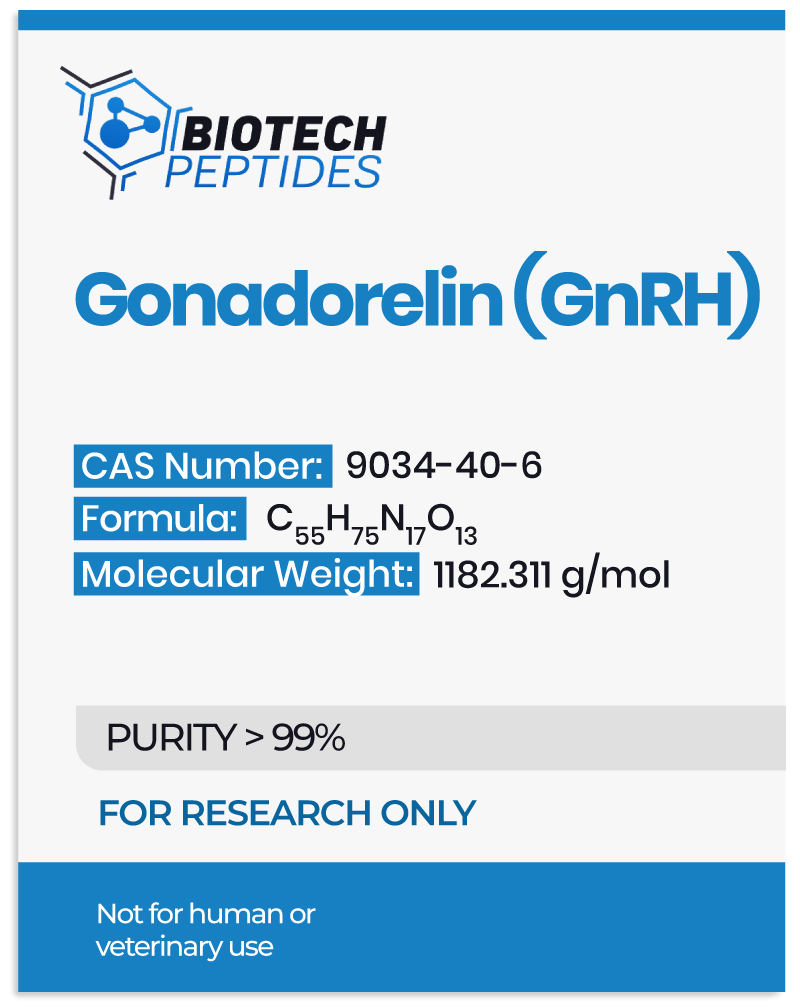
Gonadorelin is a decapeptide that may play a role in the hypothalamic-pituitary-gonadal axis. Its potential to bind to gonadotropin-releasing hormone receptors may trigger intracellular signaling pathways that regulate the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary gland.
Gonadorelin also appears to play an essential role in the estrous cycle and especially its ovulatory phase, which may be potentially due to a peak in its levels or a peak in a change in the sensitivity of the gonadotropin-releasing hormone receptors. Moreover, the presence of Gonadorelin and GnRH receptors in various brain regions suggests that it may have neuromodulatory action beyond its well-known role in gonadotropin release and the estrous cycle.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References
- Perrett, R. M., & McArdle, C. A. (2013). Molecular mechanisms of gonadotropin-releasing hormone signaling: integrating cyclic nucleotides into the network. Frontiers in endocrinology, 4, 180. https://doi.org/10.3389/fendo.2013.00180
- Casteel CO, Singh G. Physiology, Gonadotropin-Releasing Hormone. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558992/
- Maeda, K., Ohkura, S., Uenoyama, Y., Wakabayashi, Y., Oka, Y., Tsukamura, H., & Okamura, H. (2010). Neurobiological mechanisms underlying GnRH pulse generation by the hypothalamus. Brain research, 1364, 103–115. https://doi.org/10.1016/j.brainres.2010.10.026
- Marques P, Skorupskaite K, Rozario KS, et al. Physiology of GnRH and Gonadotropin Secretion. [Updated 2022 Jan 5]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279070/
- Jones, R. E., & Lopez, K. H. (2013). Human reproductive biology. Academic Press.
- Karsch, F. J., Bowen, J. M., Caraty, A., Evans, N. P., & Moenter, S. M. (1997). Gonadotropin-releasing hormone requirements for ovulation. Biology of reproduction, 56(2), 303–309. https://doi.org/10.1095/biolreprod56.2.303
- Ferré-Dolcet, L., Frumento, P., Abramo, F., & Romagnoli, S. (2021). Disappearance of signs of heat and induction of ovulation in oestrous queens with gonadorelin: a clinical study. Journal of feline medicine and surgery, 23(4), 344–350. https://doi.org/10.1177/1098612X20951284
- van Kasteren, Y. M., Hoek, A., & Schoemaker, J. (1995). Ovulation induction in premature ovarian failure: a placebo-controlled randomized trial combining pituitary suppression with gonadotropin stimulation. Fertility and sterility, 64(2), 273–278. https://doi.org/10.1016/s0015-0282(16)57722-x
- Martínez-Moreno, C. G., Calderón-Vallejo, D., Harvey, S., Arámburo, C., & Quintanar, J. L. (2018). Growth Hormone (GH) and Gonadotropin-Releasing Hormone (GnRH) in the Central Nervous System: A Potential Neurological Combinatory Therapy?. International journal of molecular sciences, 19(2), 375. https://doi.org/10.3390/ijms19020375