This pharmacological profile places Retatrutide peptide at the forefront of current peptide-based strategies. Several peptides like these have been subject to investigation into their potential impact on the modulation of adiposity and metabolic function. Preliminary findings suggest that tri-agonist activity may confer a better-supported metabolic impact relative to dual—or mono-agonist approaches.
Mechanism of Action
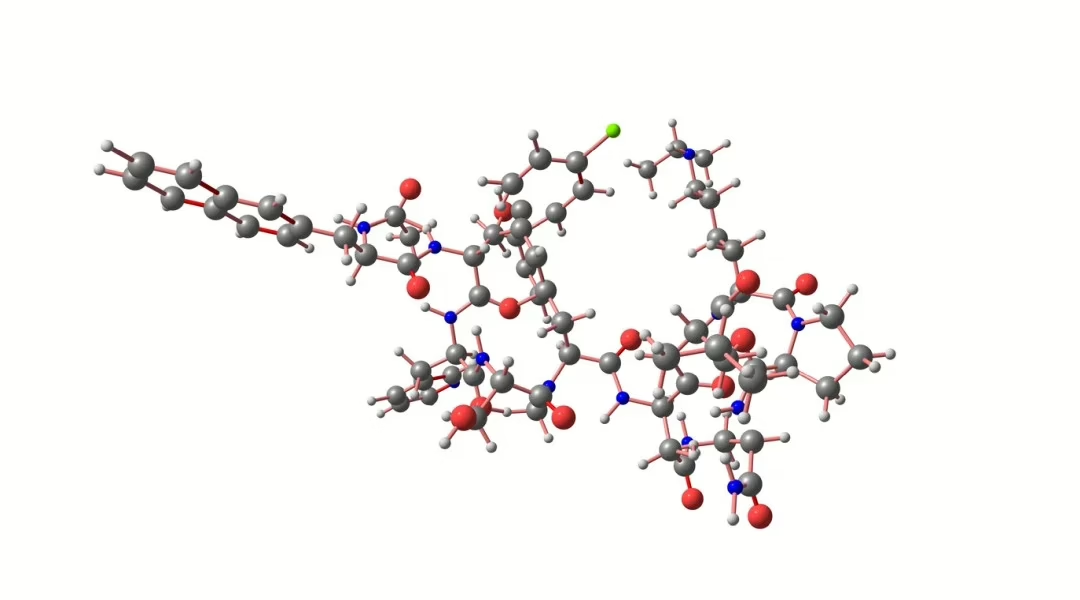
The mechanism of action of Retatrutide peptide reportedly involves coordinated receptor agonism across GLP-1R, GIPR, and GCGR pathways.[1] Activation of GLP-1R and GIPR is hypothesized to mitigate overall caloric intake via central and peripheral hunger hormone signal regulation. Concurrently, stimulation of the glucagon receptor may contribute to increased energy expenditure through hepatic and adipose tissue pathways.[1]
This dual modulation, i.e., attenuation of caloric intake alongside promoting efficient caloric utilization, may contribute in some way to significant overall mass mitigation observed in early-phase studies observing mammalian research models. Research suggests that this integrated tri-receptor engagement may result in sustained alterations in energy balance, while also being speculated to contribute to some side impacts.
Scientific Research and Studies
Retatrutide Peptide: Mass Mitigation and Excess Adiposity
A randomized, double-blind, placebo-controlled phase 2 investigation[2] aimed to review the efficacy of Retatrutide in research models displaying excess adiposity overall mass. In studies like these, there’s a particular interest in mammalian research models that are not impacted by Type 2 diabetes mellitus. In a laboratory setting over 48 weeks, research models were assigned to various Retatrutide concentrations or a placebo. The primary endpoint focused on the mean percentage change in overall mass.
When all data was collected and reviewed, the introduction of the highest concentration of peptide appeared to have resulted in a mean overall mass mitigation of 24.2%; This stands in stark contrast to a 2.1% mitigation in the placebo cohort. A graded concentration-response pattern was deemed apparent, with escalating Retatrutide concentrations reportedly yielding progressively greater mitigations in adiposity.
These outcomes support mass mitigation data reported by other researchers observing for GLP-1 mono-agonists (e.g., Semaglutide) and GLP-1/GIP dual agonists (e.g., Tirzepatide). In studies like these, achieving comparable outcomes over extended timelines is typical. The findings suggest better-supported potency via simultaneous activation of multiple metabolic hormone pathways.
Retatrutide Peptide: Research in Type 2 Diabetes Mellitus
A separate phase 2 trial[3] assessed Retatrutide’s glycemic and overall mass-related outcomes in models with established Type 2 diabetes mellitus. The cohort received titrated concentrations up to 36 weeks and was evaluated for HbA1c modulation and overall changes in mass and adiposity relative to baseline.
Data suggested a mean HbA1c mitigation of 1.8 percentage points in the higher-concentration cohorts and a concurrent mean overall mass mitigation of 16.9%. Both endpoints appeared to have achieved statistical significance relative to placebo, indicating dual metabolic relevance.
These observations reinforce the hypothesized multifactorial action of Retatrutide, which may simultaneously support insulin sensitivity and promote overall mass and adiposity mitigation through receptor-mediated mechanisms. Further trials with long-term endpoints are warranted to assess the durability of glycemic control and possible metabolic action.
Retatrutide Peptide and Non-Alcoholic Fatty Liver Disease (NAFLD)
Exploratory outcomes from the aforementioned adiposity study included imaging-based assessments of hepatic fat content that drew upon MRI-PDFF (proton density fat fraction). Research models exposed to Retatrutide in laboratory settings reportedly displayed measurable mitigations in liver fat. However, these findings were classified as secondary or exploratory endpoints pending confirmation in dedicated hepato-metabolic studies.
The underlying mechanistic hypothesis involves glucagon receptor-mediated support of hepatic lipid oxidation and suppression of gluconeogenesis, consistent with preclinical data supporting glucagon’s role in mitigating hepatic steatosis. Although preliminary and further studies are warranted, the researchers have made statements like “these findings hold promise for the development of … [mass] loss interventions in this population group.”[4]
Mechanistic Basis: GLP-1, GIP, and Glucagon Receptor Co-Agonism
Retatrutide’s pharmacodynamics profile is characterized by the co-activation of three distinct hormonal pathways, GLP-1R, GIPR, and GCG, contributing to complementary metabolic impacts.[1] GLP-1 receptor stimulation has been extensively documented to delay gastric emptying and support satiety through hypothalamic and peripheral signaling axes. GIP receptor activity, while historically controversial, appears to potentially impact GLP-1’s metabolic interactions by contributing to the modulation of insulin sensitivity and promoting adaptive adipose tissue remodeling.
Glucagon receptor activation is theorized to augment total caloric expenditure via increased lipolysis and hepatic fat oxidation, potentially reducing visceral adiposity and supporting metabolic rate. The synergistic co-engagement of these receptors represents a novel strategy in addressing excessive adiposity and other types of metabolic disorder, with implications for broader cardio-metabolic risk modulation. As per the researchers, the peptide has indicated “significant improvements in [overall mass] and metabolic outcomes among [mature research models impacted by] obesity and had an appropriate … profile.”[5]
The early-phase clinical data on Retatrutide underscore its potential as a next-generation agent for excess adiposity, type 2 diabetes, and hepatic steatosis. By leveraging triple hormone receptor agonism, Retatrutide is suggested to deliver multifaceted metabolic benefits that appear to surpass those of existing mono- or dual-agonist agents. However, the long-term durability of impact and broader relevance across diverse studies of mammalian research models have yet to be firmly established. Phase 3 trials and further mechanistic investigations will be critical to validating these findings and guiding their future relevance to scientific studies.
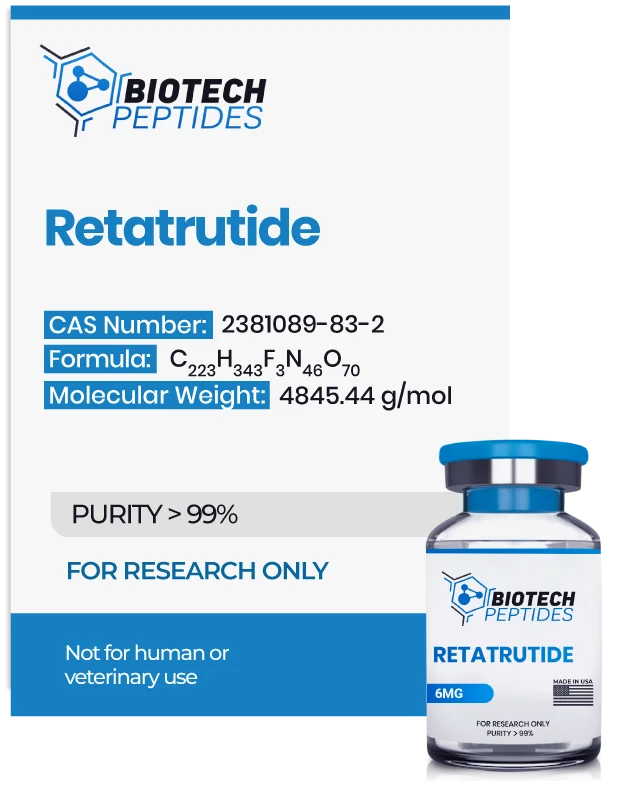
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References:
- Toufik Abdul-Rahman, Poulami Roy, Fatma Kamal Ahmed, Jann Ludwig Mueller-Gomez, Sarmistha Sarkar, Neil Garg, Victor Oluwafemi Femi-Lawal, Andrew Awuah Wireko, Hala Ibrahim Thaalibi, Muhammad Usman Hashmi, Andrew Sefenu Dzebu, Sewar Basheer Banimusa, Aayushi Sood, The power of three: Retatrutide’s role in modern obesity and diabetes therapy, European Journal of Pharmacology, Volume 985, 2024, 177095, ISSN 0014-2999, https://doi.org/10.1016/j.ejphar.2024.177095
- Ania M. Jastreboff et al., Triple–Hormone-Receptor Agonist Retatrutide for Obesity – A Phase 2 Trial, 2023, New England Journal of Medicine, P 514-526, pg. 389 doi:10.1056/NEJMoa2301972; https://www.nejm.org/doi/full/10.1056/NEJMoa2301972
- Rosenstock J, Frias J, Jastreboff AM, Du Y, Lou J, Gurbuz S, Thomas MK, Hartman ML, Haupt A, Milicevic Z, Coskun T. Retatrutide, a GIP, GLP-1 and glucagon receptor agonist, for people with type 2 diabetes: a randomised, double-blind, placebo and active-controlled, parallel-group, phase 2 trial conducted in the USA. Lancet. 2023 Aug 12;402(10401):529-544. doi: 10.1016/S0140-6736(23)01053-X. Epub 2023 Jun 26. PMID: 37385280. https://pubmed.ncbi.nlm.nih.gov/37385280/
- Kaur M, Misra S. A review of an investigational drug retatrutide, a novel triple agonist agent for the treatment of obesity. Eur J Clin Pharmacol. 2024 May;80(5):669-676. doi: 10.1007/s00228-024-03646-0. Epub 2024 Feb 17. PMID: 38367045. https://pubmed.ncbi.nlm.nih.gov/38367045/