Palmitoyl Tripeptide-5 (Syn-Coll) Peptide and Collagen Production
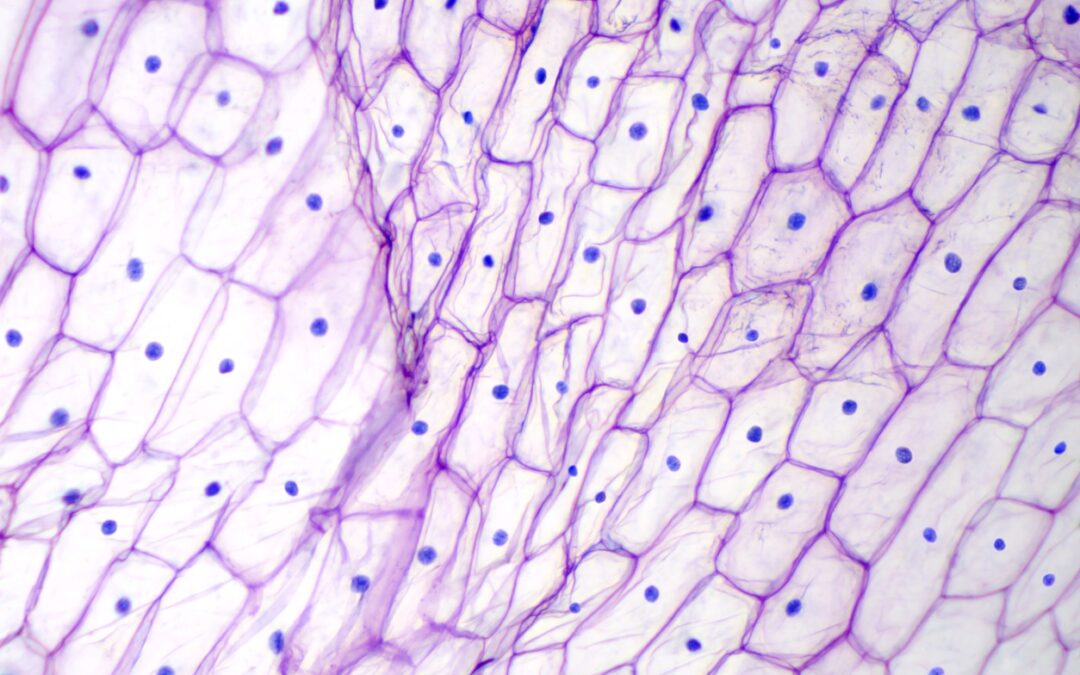
Fibroblasts are considered to be among the most commonly occurring cells in the skin. The main function of these cells appears to be the production collagen proteins. The number of active fibroblasts and levels of collagen declines naturally, potentially leading to increasing instances of creasing across the skin surface. Palmitoyl Tripeptide-5 appears to function similarly to Thrombospodin-1 to stimulate transforming growth factor-induced collagen degradation.
Functions of Palmitoyl Tripeptide-5
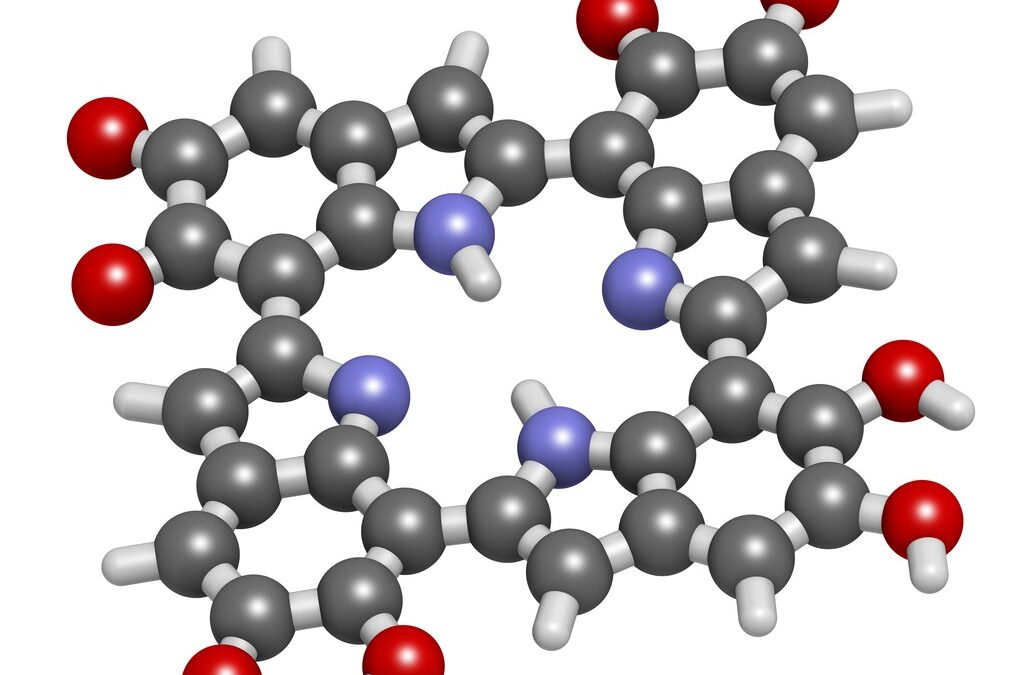
TSP-1 is a naturally occurring peptide that appears to increase TGF-𝛃 activities. Palmitoyl Tripeptide-5 appears to exhibit the same characteristics as TSP-1, increasing Type I and III collagen levels in the dermal (skin) fibroblasts.[2] The researchers noted that “Investigator assessments of both periocular and perioral wrinkles showed statistically significant improvements over Baseline within minutes of initial application; these positive findings continued to improve through Months 1 and 3.” Experimental results suggest that Syn-Coll increases Type I and III collagen levels by 2-3 folds above the normal levels.[3]
TSP-1 is considered to be an extracellular matrix (ECM) protein. It appears to cohabit with collagen and elastin in the skin. A specific part of TSP-1 is harvested for use in Palmitoyl Tripeptide-5 production. This part stimulates latent TGF-𝛃. Just like TSP-1, Syn-Coll may function to enhance tissue repair. It appears active in the post-natal development of skin structures.[4]
Palmitoyl Tripeptide-5 may also potentially deactivate matrix metalloproteinases I and III (MMP1 and MMP3). Matrix metalloproteinases are enzymes that act to degrade collagen. These enzymes may be beneficial, as they recycle collagen following cell aging, but they have been suggested to hike in conditions such as inflammation to abnormal levels.
By inhibiting MMP1 and MMP3 activity, Palmitoyl Tripeptide-5 may potentially help to prevent collagen breakdown. These hypotheses suggest that Syn-Coll may promote Type I and Type III collagen formation and inhibit collagen breakdown by the abovementioned enzymes.
In terms of wrinkle reduction, Syn-Coll has been suggested to be approximately 3.5x more effective than a placebo. According to scientists, Palmitoyl Tripeptide-5 is 60% more effective than Palmitoyl Pentapeptide.[5] Palmitoyl Tripeptide-5 has been suggested to alter the effects of photo-aging damage. Syn-Coll may also rarefy pores, potentially diminishing inconsistencies in skin texture and increasing skin elasticity and firmness. Palmitoyl Tripeptide-5 is considered to be cold-processible.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References
- Thorsen, M., Yde, B., Pedersen, U., Clauden, K. & Lawesson, S.-O. Studies on amino acids and peptides-V. Tetrahedron 39, 3429–3435 (1983).https://doi.org/10.1016/S0040-4020(01)91596-0
- Trookman, N. S., Rizer, R. L., Ford, R., Ho, E. & Gotz, V. Immediate and Long-term Clinical Benefits of a Treatment for Facial Lines and Wrinkles. J. Clin. Aesthetic Dermatol. 2, 38–43 (2009).
- Varga, J., Rosenbloom, J. & Jimenez, S. A. Transforming growth factor beta (TGF beta) causes a persistent increase in steady-state amounts of type I and type III collagen and fibronectin mRNAs in normal human dermal fibroblasts. Biochem. J. 247, 597–604 (1987).
- Murphy-Ullrich, J. E. & Poczatek, M. Activation of latent TGF-beta by thrombospondin-1: mechanisms and physiology. Cytokine Growth Factor Rev. 11, 59–69 (2000).
- Bucay, V. W. & Day, D. Adjunctive Skin Care of the Brow and Periorbital Region. Clin. Plast. Surg. 40, 225–236 (2013).