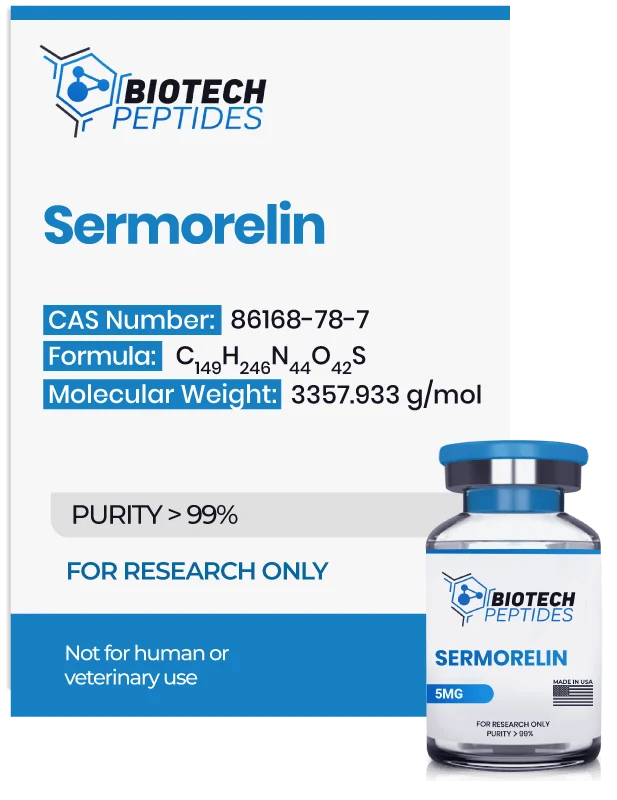
Sermorelin Overview: Growth Hormone and IGF-1 Research
The peptide was first investigated in the early 1980s following the classification of growth hormone-releasing fragments capable of stimulating pituitary-mediated signaling in mammalian research models. Early research focused on exogenous exposure of GHRF 1 to 29 amide in rodent systems, where pituitary responsiveness and somatotropic axis activation were explored under both conscious and anesthetized conditions. These foundational studies[2] contributed to broader interest in truncated GHRH analogs and their exposure in growth hormone deficiency research models.
Due to its structural mimicry of endogenous GHRH, Sermorelin has been utilized in laboratory settings to investigate hypothalamic pituitary signaling, receptor specificity, and downstream endocrine cascades. Its relatively short estimated half-life of approximately 11 to 12 minutes has also made it useful for studying pulsatile signaling dynamics within controlled experimental environments.
Contents:
- Mechanism of Action
- Scientific and Research Studies
- Sermorelin in Lipodystrophy Focused Research Models
- Anabolic-Related Research Findings
- Sermorelin and GHRH Receptor Signaling
- Growth Velocity in Experimental Models
- Sermorelin Associated Cognitive Research
- Sermorelin and Hypogonadism Related Research Models
- Sermorelin and Tumor Cell Sensitivity Research
- Clinical Studies Implying Interaction Between Growth Hormones and Thyroid
- References
Mechanism of Action
Sermorelin peptide is proposed to act through selective binding to growth hormone-releasing hormone receptors expressed on pituitary somatotroph cells. Receptor engagement is suggested to activate intracellular signaling pathways involving cyclic adenosine monophosphate and calcium-mediated second messenger systems. These pathways are commonly associated with transcriptional and secretory processes linked to growth hormone-related signaling networks.
Downstream implications observed in research models suggest modulation of insulin-like growth factor 1 signaling, a molecule frequently studied in relation to anabolic and metabolic pathways associated with growth hormone activity. Due to its apparent receptor specificity, Sermorelin has been reported to exhibit minimal interaction with other endocrine axes, including those regulating prolactin, cortisol, insulin, glucose, and thyroid hormones.
In laboratory settings, Sermorelin peptide continues to be applied as a research peptide for investigating GHRH receptor dynamics, intracellular signaling fidelity, and somatotropic axis regulation
Scientific Research and Studies
Sermorelin in Lipodystrophy Focused Research Models
Sermorelin peptide has also been evaluated in controlled research models examining lipodystrophy-associated alterations in physical composition.[3] In one placebo-controlled investigation involving 31 subjects, participants were assigned to either a Sermorelin-exposed group or a control group for a 12-week study duration. Results suggested that growth hormone-related signaling markers were significantly elevated in the peptide group when compared with placebo.
In parallel, insulin-like growth factor-1 concentrations were reported to increase, coinciding with measurable gains in lean mass. Researchers further observed statistically significant reductions in abdominal visceral fat volume and decreases in trunk to lower extremity fat distribution ratios. Importantly, no significant changes were reported in glucose or insulin-related parameters, suggesting limited involvement of broader metabolic regulatory pathways within the conditions examined.
Anabolic-Related Research Findings
Multiple research investigations have examined the relationship between Sermorelin peptide exposure and growth hormone-associated signaling outcomes. In one experimental study, mean growth hormone concentrations were reported to increase by approximately 82 percent, with signaling activity persisting for close to two hours following stimulation. These findings suggest a transient but measurable activation of somatotropic signaling pathways.
A separate longitudinal investigation[5] conducted over 16 weeks proposed more pronounced changes in growth hormone-related markers, with reported increases exceeding 100 percent. The same study suggested an approximate 28 percent elevation in circulating insulin-like growth factor 1 concentrations. Downstream observations included a statistically significant increase in lean mass, estimated at 1.26 kg, while fat mass measurements remained largely unchanged. Investigators attributed these outcomes to upgraded growth hormone-driven anabolic signaling, potentially mediated through IGF-1-related pathways. Additional reported findings included significant increases in dermal thickness, indicating broader tissue-level structural responses.
Sermorelin Peptide and GHRH Receptor Signaling
Sermorelin peptide is proposed to interact selectively with growth hormone-releasing hormone receptors through receptor-mediated molecular mechanisms that initiate intracellular signal transduction. Upon receptor engagement, structural conformational changes in the GHRH receptor are hypothesized to occur, potentially facilitating activation of downstream signaling pathways associated with somatotropic regulation. These interactions have been examined primarily within controlled in vitro systems and preclinical models.[6]
One proposed mechanism involves stimulation of adenylate cyclase activity following receptor binding. This process is suggested to increase intracellular concentrations of cyclic adenosine monophosphate through conversion of adenosine triphosphate. Elevated cAMP levels are commonly associated with activation of protein kinase A (PKA), an enzyme that regulates multiple downstream signaling targets through phosphorylation events. Activation of the cAMP PKA pathway is thought to modulate transcriptional and secretory processes within pituitary somatotroph cells.
Through these signaling cascades, Sermorelin-associated receptor activation is hypothesized to support regulated growth hormone release patterns. Subsequent downstream signaling is believed to involve modulation of insulin-like growth factor 1 synthesis, a molecule frequently studied for its role in growth hormone-related anabolic and tissue remodeling pathways. These mechanisms continue to be explored as part of broader investigations into GHRH receptor dynamics and endocrine signaling specificity.
Growth Velocity in Experimental Models
Research[1] examining growth-related outcomes has investigated Sermorelin signaling within models of idiopathic growth hormone deficiency. In underdeveloped animal systems, exposure to Sermorelin-associated signaling was reported to correlate with increased growth velocity and longitudinal growth parameters over a 12-month observational period. These changes were proposed to reflect sustained activation of growth hormone-related pathways rather than transient signaling implications.
Extended follow-up analyses suggested that elevated growth velocity indicators persisted for an average duration of up to 36 months following continuous experimental exposure. Researchers hypothesized that these prolonged effects may be linked to adaptive changes within the somatotropic axis, including receptor responsiveness and downstream transcriptional regulation. Such findings have contributed to ongoing interest in Sermorelin as a research tool for studying growth regulation and endocrine adaptability in deficiency models.
Sermorelin Peptide Associated Cognitive Research
Research conducted in the early 2000s explored potential associations between cellular age-related reductions in growth hormone signaling and changes in cognitive performance. In one investigation involving 89 older mammalian research , researchers examined whether attenuated somatotropic activity might correlate with measurable alterations in cognitive function. Cellular age-associated declines in growth hormone signaling have been hypothesized to modulate multiple physiological systems, including neural processes involved in information acquisition, processing, and memory consolidation.
Following experimental exposure to Sermorelin-associated signaling, investigators reported refinements across several standardized cognitive assessment parameters. Performance gains were observed in select components of the Wechsler Adult Intelligence Scale, including picture arrangement and verbal reasoning measures. These findings among mammalian research models studied were interpreted as suggestive of a potential link between growth hormone-related signaling pathways and cognitive performance metrics, though underlying mechanisms remain an area of ongoing investigation.
Sermorelin and Hypogonadism Related Research Models
Early experimental investigations[8] examining Sermorelin-associated signaling have explored its relationship with lean mass regulation and gonadotropic hormone dynamics. One study evaluated whether growth hormone-releasing hormone analog activity might modulate endocrine patterns commonly associated with hypogonadal models, which are frequently characterized by increased adiposity. In this investigation, mammalian research models were divided into two groups receiving sequential exposure to Sermorelin and a longer GHRH analog, GHRH 1 to 40, given in alternating order with a one-week interval.
Researchers reported that, irrespective of sequence, Sermorelin-associated signaling appeared to coincide with increased release of follicle-stimulating hormone and luteinizing hormone. These observations led to the hypothesis that GHRH receptor activation may indirectly modulate gonadotropic hormone regulation, with potential downstream implications for androgen-related signaling pathways.
Subsequent investigations expanded this line of inquiry in a controlled study involving 19 male subjects across two age cohorts. Nine participants were between 22 and 33 years of age, while ten were between 60 and 78 years of age. The older cohort was exposed to two different Sermorelin concentrations across two 28-day experimental periods, separated by a 14-day interval. Researchers reported modest elevations in testosterone-associated signaling markers in the older group, though these changes did not reach statistical significance.
Additional observations suggested that growth hormone-related signaling exhibited diurnal variation, with higher activity reported during nocturnal periods compared to daytime measurements across age groups. These findings have contributed to ongoing research examining interactions between somatotropic and gonadotropic endocrine axes under controlled experimental conditions.
Sermorelin Peptide and Tumor Cell Sensitivity Research
Sermorelin peptide has also been examined within experimental mammalian screening models. In one large-scale investigation, 1,018 glioma-derived samples were exposed to a library of more than 4,000 compounds, with a drug response score generated for each compound sample pairing. Within this screening framework, Sermorelin was reported to elicit one of the highest sensitivity responses across the evaluated samples.
Subsequent analyses[9] suggested that the observed sensitivity may be associated with interference in tumor cell cycle progression. Researchers hypothesized that Sermorelin-related signaling may modulate regulatory mechanisms involved in cellular proliferation, potentially contributing to cell cycle arrest under laboratory conditions. These findings have prompted further investigation into GHRH-related peptide interactions within tumor biology models, though mechanistic interpretations remain exploratory.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References:
- Prakash, A, and K L Goa. “Sermorelin: a review of its use in the diagnosis and treatment of children with idiopathic growth hormone deficiency.” BioDrugs: clinical immunotherapeutics, biopharmaceuticals and gene therapy vol. 12,2 (1999): 139-57. https://pubmed.ncbi.nlm.nih.gov/18031173/
- Clark, R G, and I C Robinson. “Growth induced by pulsatile infusion of an amidated fragment of hGH releasing factor in normal and GHRF-deficient rats.” Nature vol. 314, 6008 (1985): 281-3. https://pubmed.ncbi.nlm.nih.gov/2858818/
- Koutkia, Polyxeni et al. “Growth hormone-releasing hormone in HIV-infected men with lipodystrophy: a randomized controlled trial.” JAMA vol. 292,2 (2004): 210-8. https://pubmed.ncbi.nlm.nih.gov/15249570/
- Vittone, J., Blackman, M. R., Busby-Whitehead, J., Tsiao, C., Stewart, K. J., Tobin, J., Stevens, T., Bellantoni, M. F., Rogers, M. A., Baumann, G., Roth, J., Harman, S. M., & Spencer, R. G. (1997). Effects of single nightly injections of growth hormone-releasing hormone (GHRH 1-29) in healthy elderly men. Metabolism: clinical and experimental, 46(1), 89–96. https://doi.org/10.1016/s0026-0495(97)90174-8
- Khorram, O., Laughlin, G. A., & Yen, S. S. (1997). Endocrine and metabolic effects of long-term administration of [Nle27]growth hormone-releasing hormone-(1-29)-NH2 in age-advanced men and women. The Journal of clinical endocrinology and metabolism, 82(5), 1472–1479. https://doi.org/10.1210/jcem.82.5.3943
- Zhou, F., Zhang, H., Cong, Z., Zhao, L. H., Zhou, Q., Mao, C., Cheng, X., Shen, D. D., Cai, X., Ma, C., Wang, Y., Dai, A., Zhou, Y., Sun, W., Zhao, F., Zhao, S., Jiang, H., Jiang, Y., Yang, D., Eric Xu, H., … Wang, M. W. (2020). Structural basis for activation of the growth hormone-releasing hormone receptor. Nature communications, 11(1), 5205. https://doi.org/10.1038/s41467-020-18945-0
- Vitiello, Michael V et al. “Growth hormone releasing hormone improves the cognition of healthy older adults.” Neurobiology of aging vol. 27,2 (2006): 318-23. https://pubmed.ncbi.nlm.nih.gov/16399214/
- Sinha, Deepankar K et al. “Beyond the androgen receptor: the role of growth hormone secretagogues in the modern management of body composition in hypogonadal males.” Translational andrology and urology vol. 9,Suppl 2 (2020): S149-S159. doi:10.21037/tau.2019.11.30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7108996/
- Chang, Yuanhao et al. “A potentially effective drug for patients with recurrent glioma: sermorelin.” Annals of translational medicine vol. 9,5 (2021): 406. doi:10.21037/atm-20-6561. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8033379/