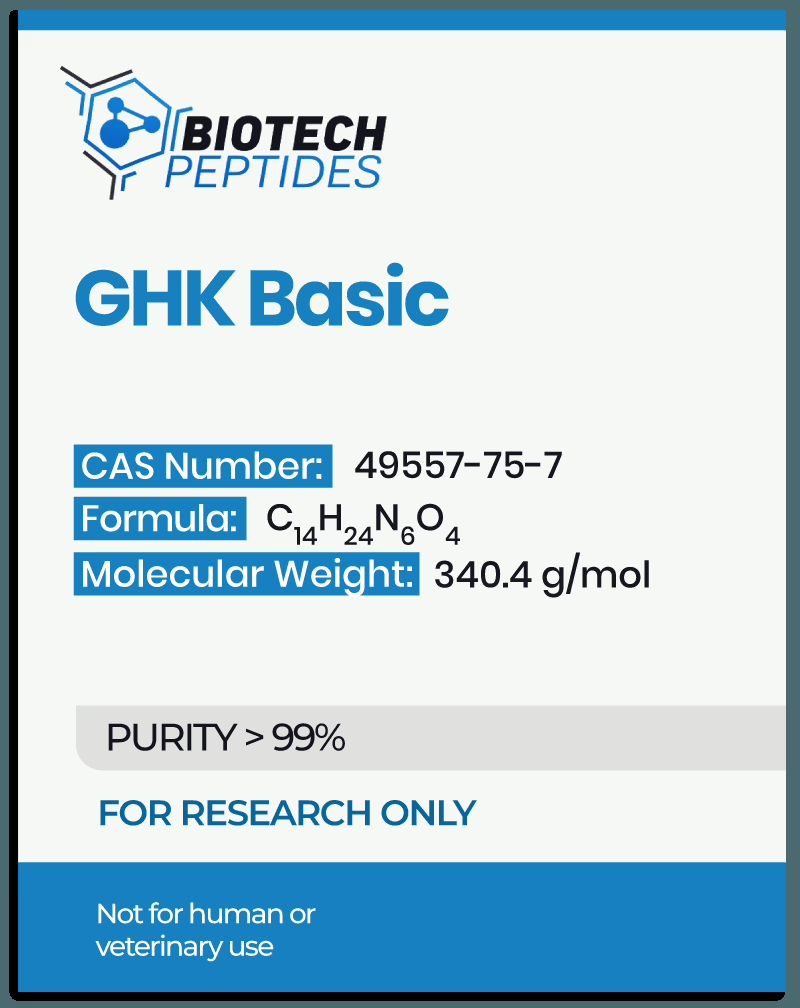
Tripeptide-1: Antioxidant, Anti-Inflammatory, and Regenerative Research
GHK is believed to represent an endogenous signaling motif with roles in extracellular matrix (ECM) remodeling, tissue maintenance, and repair. Fragmentation of larger proteins, such as type I collagen, under physiological or pathological conditions, may yield GHK-containing motifs that act as regulatory peptides. Studies have proposed that its presence in localized tissue environments correlates with regenerative processes and cellular homeostasis.
The biochemical activity of Tripeptide-1 appears to be multifaceted, involving interactions with both extracellular and intracellular targets.
One proposed mechanism includes its potential as a metal-binding peptide, particularly in chelating copper ions to form a GHK-Cu²⁺ complex.[1] This complex may serve as a cofactor modulator, potentially affecting the activity of metalloproteinase, antioxidant enzymes, and other copper-dependent proteins. For example, modulation of matrix metalloproteinase (MMPs) could influence ECM degradation and remodeling, while interactions with superoxide dismutase enzymes may indirectly affect oxidative stress signaling.
Tripeptide-1 may also act at the genomic level. Research suggests that the GHK moiety may alter gene expression profiles by influencing transcriptional regulators and epigenetic mediators. Preliminary studies suggest upregulation of genes associated with tissue regeneration, anti-inflammatory signaling, and antioxidant response pathways. Simultaneously, a downregulation of genes related to fibrosis and oxidative damage has been proposed, though the precise signaling cascades remain under investigation.
Another suggested mechanism involves modulation of cellular adhesion and communication pathways. Tripeptide-1 might affect integrin signaling and influence the expression of surface receptors that regulate cellular migration, differentiation, and proliferation. Through these interactions, it may contribute to re-establishing structural and functional integrity in damaged or tissues experiencing cellular aging.
Scientific Research and Studies
Tripeptide-1 and Collagen Homeostasis
Researchers suggest there may be a “presence of a Tripeptide-1 triplet in the alpha 2(I) chain of type I collagen”, specifically in residues 853-855.[1] This sequence overlap has led to the hypothesis that proteolytic cleavage of mature collagen fibers may liberate GHK-containing fragments into the extracellular matrix. These fragments may act as matricryptic signals, potentially influencing resident fibroblasts to initiate reparative collagen synthesis in response to tissue degradation.
One proposed mechanism involves Tripeptide-1 functioning as a molecular analog of native collagen degradation products while concurrently chelating copper ions. This peptide-metal complex may facilitate cellular copper uptake, thereby influencing intracellular enzyme systems dependent on this metal. Specifically, fibroblast-derived lysyl oxidase and other copper-requiring enzymes involved in collagen maturation may exhibit altered activity following such uptake. Rather than supporting amino acid substrate availability, research suggests that Tripeptide-1 may influence post-translational enzymatic activity, including the regulation of prolyl and lysyl hydroxylases implicated in collagen cross-linking and stability.
Findings reported by another study[2] further explore the regulatory dynamics between Tripeptide-1 and matrix metalloproteinase (MMPs). In controlled models exhibiting ECM degradation, Tripeptide-1 exposure was associated with modulated expression of pro-MMP-2 and pro-MMP-9, as well as a corresponding reduction in their active forms. Although MMPs are required for matrix remodeling and cellular motility, excess enzymatic activity may result in excessive collagen turnover, potentially disrupting matrix regeneration.
The observed reduction in MMP activity following Tripeptide-1 exposure may suggest a modulatory role in the extracellular proteolytic environment. This peptide may help maintain a protease balance conducive to orderly collagen deposition, fibril assembly, and stabilization of nascent ECM structures. Additionally, decreased degradation of provisional matrix proteins such as fibronectin and laminin may support fibroblast adhesion and microvascular organization, both of which are considered essential to early-stage repair mechanisms.
Tripeptide-1 and Wound Recovery in Controlled Research Models
Research into Tripeptide-1 has highlighted its potential roles in tissue regeneration, particularly within experimental wound healing paradigms.
In studies involving diabetic wound models, the copper-complexed form of Tripeptide-1 was incorporated into structured wound care protocols. Results posed that models receiving this peptide exhibited increased closure rates in plantar ulcers when compared to control groups. Reports also noted a reduced incidence of microbial contamination in these lesions, suggesting a possible impact on the local inflammatory microenvironment and barrier restoration mechanisms.[3]
In additional preclinical investigations using rabbit wound models, Tripeptide-1 was speculated to be associated with enhanced granulation tissue formation. Histological analyses suggest elevated neutrophil and microvascular densities in the peptide-exposed group, particularly during the early and mid-stages of wound closure. These observations may suggest accelerated cellular infiltration and vascular remodeling, which are deemed integral to effective tissue repair. The researchers hypothesized that increased antioxidant enzyme activity might underlie some of the observed interactions, particularly those related to oxidative damage attenuation.[4]
Further investigations in ischemic wound models appeared to show reductions in key pro-inflammatory markers, including tumor necrosis factor-alpha (TNF-α), MMP-2, and MMP-9, following Tripeptide-1 exposure.[2] These biomolecules are commonly associated with prolonged inflammation and matrix degradation, suggesting that Tripeptide-1 may modulate proteolytic and inflammatory responses in impaired healing environments.
Subsequent studies utilizing murine models under both standard and diabetic conditions incorporated GHK-functionalized collagen dressings. These peptide-enriched films appeared to yield increased wound closure percentages by the third week of observation. The exposed wounds also seemed to exhibit elevated levels of glutathione and ascorbic acid, both of which are deemed by scientists to be critical redox-active molecules that support epithelial regeneration and fibroblast activity. Morphological data suggested accelerated epithelialization, fibroblast proliferation, and potential stimulation of collagen deposition. These findings may support the hypothesis that Tripeptide-1 contributes to multiple stages of cutaneous tissue recovery, including ECM synthesis, vascularization, and epidermal barrier reformation.
Tripeptide-1 and Skin Structure Modulation
Tripeptide-1 has been studied for its role in modulating extracellular matrix (ECM) components critical to dermal structure and resilience. The peptide’s sequence corresponds to a collagen-derived fragment that may arise during proteolytic degradation. This similarity has prompted investigations into its role as a regulatory signal influencing fibroblast behavior.
Studies suggest that Tripeptide-1 exposure may stimulate fibroblasts to increase production of collagen, elastin, and glycosaminoglycan, which are considered to be key macromolecules required for mechanical strength, elasticity, and hydration of the dermal matrix.[1]
In controlled research environments, Tripeptide-1 appeared to be associated with increased proliferation of dermal keratinocytes and apparent improvements in skin hydration and elasticity. These effects may result from enhanced biosynthesis of type I collagen and remodeling of the dermal ECM. Skin explants exposed to Tripeptide-1 reportedly yielded increased skin thickness and smoother surface morphology under certain experimental parameters.[5]
In a separate investigation involving post-laser resurfacing models, Tripeptide-1 was included in post-procedure observations to evaluate its impact on recovery. While both the peptide and control groups exhibited general improvements in skin appearance, models receiving Tripeptide-1 enriched formulations appeared to express increased results, indicating the possible supportive effects of the compound during the recovery phase of dermal procedures.[6]
Tripeptide-1 and UVB-Induced Oxidative Stress Defense
Under ultraviolet B (UVB) exposure, epidermal cells may accumulate reactive carbonyl species (RCS) and reactive oxygen species (ROS), both of which contribute to cytotoxic damage and structural protein modification. Laboratory findings suggest that Tripeptide-1 may provide indirect antioxidant support by quenching RCS and thereby reducing the metabolic demand on glutathione (GSH), a primary intracellular redox buffer.[7]
Murine keratinocyte cultures preconditioned with Tripeptide-1 prior to UVB exposure appeared to show lower extracellular levels of GSH-RCS conjugates, suggesting partial peptide-mediated detoxification of reactive aldehydes such as 4-hydroxynonenal (HNE) and acrolein. This sparing of GSH may contribute to preserved redox homeostasis and mitochondrial viability.
Furthermore, Tripeptide-1 appears to help sustain the function of superoxide dismutase (SOD) in oxidative conditions by mitigating its glycation. This may occur through preferential binding of Tripeptide-1 to reactive aldehydes like glyoxal and methylglyoxal, which are considered to inactivate SOD and promote the formation of advanced glycation end-products (AGEs). Preservation of SOD activity may contribute to reduced accumulation of superoxide radicals and downstream nitrative stress, such as peroxynitrite-mediated protein tyrosine nitration.
Collectively, the findings suggest that Tripeptide-1 may be able “to help the [endogenous] protection of cells (GSH) to mitigate the damage of RCS and UVB radiation and acts as a scavenger of specific RCS (HNE, acrolein) and mitigates glycation of protein, avoiding the formation of advanced glycation end-products.”[7]
Tripeptide-1 and Redox-Inflammatory Modulation
Mechanistic observations propose that Tripeptide-1 may modulate iron metabolism in damaged tissues. Specifically, the peptide may inhibit iron release from ferritin, a key catalyst in lipid peroxidation reactions. In cellular models exposed to Tripeptide-1, it appeared to show a substantial reduction in iron efflux, potentially through steric interactions at ferritin channel sites.[8] By limiting free iron availability, the peptide may attenuate iron-mediated oxidative amplification and the associated inflammatory cascades.
In murine models of lipopolysaccharide-induced acute lung injury, Tripeptide-1 seemed to be linked to reductions in inflammatory cytokines and oxidative stress markers. The peptide was reported to decrease TNF-α and IL-6 concentrations while enhancing the expression of endogenous antioxidant enzymes. These purported effects were accompanied by a proposed downregulation of NF-κB and p38 MAPK signaling pathways, which are frequently implicated in inflammatory gene transcription.[9]
Further studies[10] in alveolar epithelial models suggest an upregulation of Nrf2 expression following Tripeptide-1 exposure. Nrf2 is a transcription factor central to the regulation of antioxidant defenses, and its activation may contribute to improved cellular resistance to exogenous oxidative stressors. Comparative studies also suggest that Tripeptide-1 may exhibit stronger reactivity with hydroxyl radicals than other endogenous peptides, including carnosine and reduced glutathione, under matched experimental conditions.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References:
- Maquart, F. X., Pickart, L., Laurent, M., Gillery, P., Monboisse, J. C., & Borel, J. P. (1988). Stimulation of collagen synthesis in fibroblast cultures by the tripeptide-copper complex glycyl-L-histidyl-L-lysine-Cu2+. FEBS letters, 238(2), 343–346. https://doi.org/10.1016/0014-5793(88)80509-x
- Canapp, S. O., Jr, Farese, J. P., Schultz, G. S., Gowda, S., Ishak, A. M., Swaim, S. F., Vangilder, J., Lee-Ambrose, L., & Martin, F. G. (2003). The effect of topical tripeptide-copper complex on the healing of ischemic open wounds. Veterinary surgery: VS, 32(6), 515–523. https://doi.org/10.1111/j.1532-950x.2003.00515.x
- Mulder, G. D., Patt, L. M., Sanders, L., Rosenstock, J., Altman, M. I., Hanley, M. E., & Duncan, G. W. (1994). Enhanced healing of ulcers in patients with diabetes by treatment with glycyl-l-histidyl-l-lysine copper. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society, 2(4), 259–269. https://doi.org/10.1046/j.1524-475X.1994.20406.x
- Gul, N. Y., Topal, A., Cangul, I. T., & Yanik, K. (2008). The effects of tripeptide copper complex and helium-neon laser on wound healing in rabbits. Veterinary dermatology, 19(1), 7–14. https://doi.org/10.1111/j.1365-3164.2007.00647.x
- Abdulghani, A. A., Sherr, A., Shirin, S., Solodkina, G., Tapia, E. M., Wolf, B., & Gottlieb, A. B. (1998). Effects of creams containing vitamin C, a copper-binding peptide cream and melatonin compared with tretinoin on the ultrastructure of normal skin-A pilot clinical, histologic, and ultrastructural study. Disease Management and Clinical Outcomes, 4(1), 136-141.
- Miller, T. R., Wagner, J. D., Baack, B. R., & Eisbach, K. J. (2006). Effects of copper tripeptide complex on CO2 laser-resurfaced skin. Archives of facial plastic surgery, 8(4), 252–259. https://doi.org/10.1001/archfaci.8.4.252
- Cebrián, J., Messeguer, A., Facino, R. M., & García Antón, J. M. (2005). New anti-RNS and -RCS products for cosmetic treatment. International journal of cosmetic science, 27(5), 271–278. https://doi.org/10.1111/j.1467-2494.2005.00279.x
- Miller, D. M., DeSilva, D., Pickart, L., & Aust, S. D. (1990). Effects of glycyl-histidyl-lysyl chelated Cu(II) on ferritin dependent lipid peroxidation. Advances in experimental medicine and biology, 264, 79–84. https://doi.org/10.1007/978-1-4684-5730-8_11
- Park, J. R., Lee, H., Kim, S. I., & Yang, S. R. (2016). The tri-peptide GHK-Cu complex ameliorates lipopolysaccharide-induced acute lung injury in mice. Oncotarget, 7(36), 58405–58417. https://doi.org/10.18632/oncotarget.11168
- Zhang, Q., Yan, L., Lu, J., & Zhou, X. (2022). Glycyl-L-histidyl-L-lysine-Cu2+ attenuates cigarette smoke-induced pulmonary emphysema and inflammation by reducing oxidative stress pathway. Frontiers in molecular biosciences, 9, 925700. https://doi.org/10.3389/fmolb.2022.925700