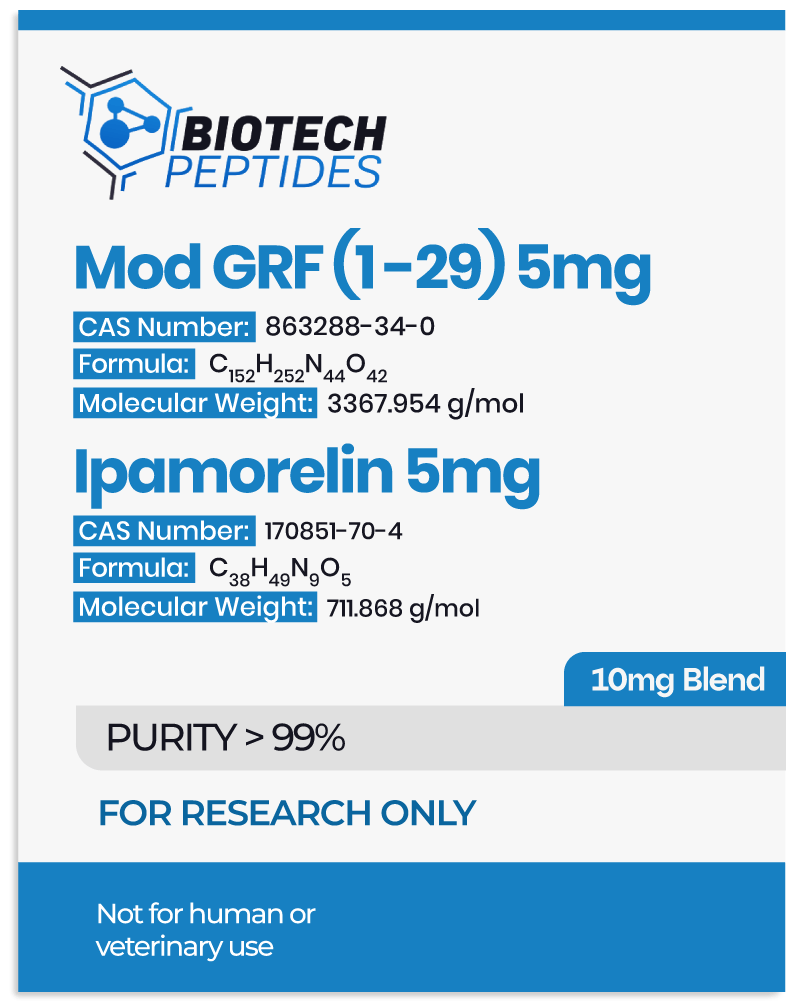
Modified GRF 1-29 & Ipamorelin Blend: Studies in Growth Hormone Secretion and Metabolic Regulation
Modified GRF 1-29, a stabilized analog of growth hormone-releasing hormone (GHRH), is reportedly designed to increase growth hormone release by targeting GHRH receptors on somatotroph cells in the anterior pituitary gland.[1] Its structural modifications, which replace four amino acids in the native sequence, are speculated to confer enhanced stability and bioavailability, potentially making it more resistant to enzymatic degradation.
Ipamorelin, a synthetic pentapeptide and selective growth hormone secretagogue (GHS), is suggested to operate by mimicking the action of ghrelin, a naturally occurring hormone involved in hunger signaling and growth hormone release. By activating growth hormone secretagogue receptor 1-alpha (GHS-R1a) in the pituitary, Ipamorelin reportedly initiates intracellular signaling pathways that stimulate the secretion of growth hormone while maintaining high selectivity to avoid affecting other hormones such as cortisol or prolactin.
Together, these peptides are speculated to offer a powerful mechanism of action where Ipamorelin may provide rapid, short-term stimulation of growth hormone release, while Modified GRF 1-29 may ensure a more sustained response by activating complementary signaling pathways. This dual-action mechanism, achieved through distinct receptor interactions, might create an extended-release profile that researchers suggest may lead to increased growth hormone activity compared to studying either peptide alone.[2]
Contents:
- Scientific and Research Studies
- Modified GRF 1-29 & Ipamorelin Blend and Growth Hormone
- Modified GRF 1-29 & Ipamorelin Blend and Cardiac Function
- Modified GRF 1-29 & Ipamorelin Blend and Potency
- Modified GRF 1-29 & Ipamorelin Blend and the Pituitary
- Gastrointestinal System
- Modified GRF 1-29 & Ipamorelin Blend and Appetite Regulation
- Modified GRF 1-29 & Ipamorelin Blend and Bone Density
- References
Scientific Research and Studies
Modified GRF 1-29 & Ipamorelin Blend and Growth Hormone
A series of studies[3] conducted in 1998 appears to provide critical insights into the function of the Modified GRF 1-29 and Ipamorelin blend in the function of growth hormone secretion. Experimental models, including rat pituitary glands, anesthetized rats, and conscious swine, were utilized to evaluate the peptides’ activity. Findings suggest that both Modified GRF 1-29 and Ipamorelin may act as agonists of GHRP-like receptors, binding to these targets to reportedly stimulate significant increases in growth hormone secretion. It also appears that the peptides exhibited high receptor specificity. While other growth hormone secretagogues often triggered elevations in additional hormones such as cortisol and ACTH, Ipamorelin and Modified GRF 1-29 “very surprisingly, did not [appear to] release ACTH or cortisol in levels significantly”, reportedly even at significantly high concentrations compared to other similar peptides.
Further research in 1999 sought to extend these findings through clinical trials. In this study,[4] eight research models were introduced with growth hormone secretagogues at progressively increasing concentrations, with amounts adjusted every 15 minutes over a two-hour period. Based on the results, it was suggested that there was a marked elevation in circulating growth hormone levels throughout the study duration, suggesting a concentration-dependent response to the blend.
These findings support the hypothesis that the combination of Modified GRF 1-29 and Ipamorelin may provide a synergistic and sustained increase of growth hormone release, laying the groundwork for future research into their potential.
Cardiac Function
In a pilot study,[5] experimental models were introduced with growth hormone-releasing hormone (GHRH) peptide analogs, including Modified GRF 1-29, to evaluate their potential effects on cardiac function. Findings from this research suggest that the peptides may positively influence myocardial function, particularly in models of myocardial infarction. The study hypothesized that Modified GRF 1-29 might enhance cardiac performance by increasing heart rate and improving blood pumping efficiency.
Modified GRF 1-29 & Ipamorelin Blend and Potency
Preliminary investigations have provided significant hypotheses into the potency of the Modified GRF 1-29 and Ipamorelin blend, specifically its potential compared to regular GRF 1-29. In one study,[6] experimental rats were exposed to GHRH peptide analogs, including Modified GRF 1-29. Results suggested that the synthetic analog may have greater efficacy in stimulating growth hormone release than its unmodified counterpart. This enhanced potency appears to be attributed to the structural modifications in Modified GRF 1-29, which may improve its stability and receptor binding efficiency, allowing for sustained biological activity over time.
Modified GRF 1-29 & Ipamorelin Blend and the Pituitary
The efficacy of the blend in promoting growth hormone secretion is closely linked to its interaction with GHRH receptors on somatotroph cells in the anterior pituitary gland. The binding of the peptide to these receptors is hypothesized to act as a catalyst for a cascade of intracellular signaling events. One such pathway involves the activation of adenylyl cyclase, which converts ATP into cyclic adenosine monophosphate (cAMP). The elevation of cAMP levels activates protein kinase A (PKA), leading to the phosphorylation of proteins, such as voltage-dependent calcium channels on the somatotroph cell membrane.[7] This phosphorylation facilitates calcium ion influx, which reportedly initiates the secretion of growth hormone from the cell’s secretory vesicles into the bloodstream.
Similarly, Ipamorelin appears to function with a distinct mechanism of action by selectively targeting the GHS-R1a receptors in the anterior pituitary. The peptide supposedly interacts with the N-terminal region of these receptors through hydrogen bonding and van der Waals forces, inducing conformational changes that activate intracellular G-protein signaling pathways. Specifically, GHS-R1a is thought to couple with Gαq/11 subunits, which subsequently activate phospholipase C (PLC). PLC cleaves phosphatidylinositol 4, 5-bisphosphate (PIP2) into two critical secondary messengers: inositol trisphosphate (IP3) and diacylglycerol (DAG). IP3 binds to receptors on the endoplasmic reticulum, prompting the release of calcium ions (Ca2+), which, in turn, reportedly activates downstream proteins that regulate growth hormone secretion.[8]
Modified GRF 1-29 & Ipamorelin Blend and the Gastrointestinal System
In a recent investigation, the potential influence of Ipamorelin on gastric motility was examined, with particular emphasis on its capacity to expedite gastric emptying. The study utilized a specialized technique to assess gastric emptying by quantifying the percentage of radioactivity remaining in the stomach 15 minutes following the introduction of a radiolabeled substance via intragastric gavage. The researchers observed that surgical manipulation of the abdominal region may have contributed to a delayed gastric emptying rate, as reported by the researchers in the control group, which received a vehicle substance. In contrast, Ipamorelin appeared to significantly accelerate the gastric emptying process relative to the control group, suggesting that Ipamorelin may potentially increase the rate of gastric emptying.
Subsequent analyses studied the possible effect of Ipamorelin on the contractile activity of gastric smooth muscle, which was induced by both acetylcholine and electrical field stimulation. The results suggested that surgical intervention and manipulation of the gastrointestinal tract in these animal models may markedly attenuate the contractile responses of gastric smooth muscle to these stimuli. Notably, this suppression appeared to be reversed when both Ipamorelin and ghrelin were co-introduced, hinting that Ipamorelin may not only facilitate gastric smooth muscle contractility but also potentially mitigate any inhibitory effects induced by certain surgical interventions.[9]
Modified GRF 1-29 & Ipamorelin Blend and Appetite Regulation
The potential effects of Ipamorelin on ghrelin receptors suggest a potential for appetite support and subsequent weight increase In a controlled study,[10] experimental models reportedly “induced a small (15%) increase in body weight by 2 weeks” following peptide exposure. Researchers propose that this compound may have disproportionately increased fat pad mass relative to total body mass, which may lead to a discernible rise in fat as measured by dual-energy X-ray absorptiometry (DEXA). Further data indicated that Ipamorelin may have elevated serum leptin levels, a hormone associated with energy balance and appetite regulation. This observation has led to the hypothesis that increased food intake may play a role in the observed weight gain in the Ipamorelin-exposed research models. The researchers suggest that growth hormone secretagogues (GHSs), such as Ipamorelin, may contribute to fat cell accumulation via mechanisms independent of growth hormone, potentially including an increase in caloric consumption.
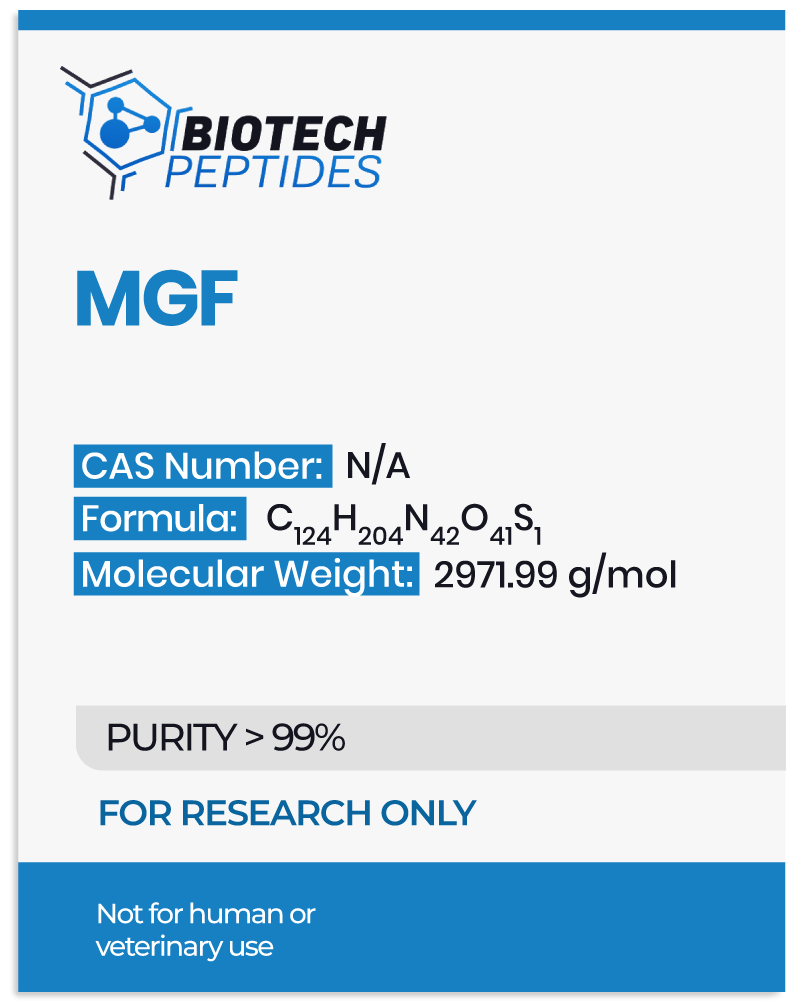
Modified GRF 1-29 & Ipamorelin Blend and Bone Density
In a study conducted with murine models, the effects of Ipamorelin on bone mass were evaluated through the introduction of both Ipamorelin and a control substance. Real-time DEXA was utilized to monitor alterations in bone mineral content, focusing on specific regions such as the femur and L6 vertebrae. Upon completion of the experimental period, mid-diaphyseal peripheral quantitative computed tomography (pQCT) scans were performed on the femurs of the models under observation. Preliminary findings suggest that Ipamorelin may be associated with an increase in weight and a potential rise in bone mineral content (BMC) in the tibia and vertebrae, as indicated by DEXA results when compared to the control group. Moreover, pQCT data point to an increase in cortical BMC, likely due to an expansion of the bone’s cross-sectional area. The researchers also hypothesize that minor stimulatory effects on linear bone growth may not have been statistically significant in the growth hormone (GH) and Ipamorelin-exposed cohorts, potentially due to the scope of the study.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References:
- The Discovery of Growth Hormone-Releasing Hormone: An Update https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2826.2008.01740.x
- Gobburu JV, Agersø H, Jusko WJ, Ynddal L. Pharmacokinetic-pharmacodynamic modeling of ipamorelin, a growth hormone releasing peptide, in human volunteers. Pharm Res. 1999 Sep;16(9):1412-6. doi: 10.1023/a:1018955126402. PMID: 10496658. https://pubmed.ncbi.nlm.nih.gov/10496658/
- Raun K, Hansen BS, Johansen NL, Thøgersen H, Madsen K, Ankersen M, Andersen PH. Ipamorelin, the first selective growth hormone secretagogue. Eur J Endocrinol. 1998 Nov;139(5):552-61. doi: 10.1530/eje.0.1390552. PMID: 9849822. https://pubmed.ncbi.nlm.nih.gov/9849822/
- Gobburu JV, Agersø H, Jusko WJ, Ynddal L. Pharmacokinetic-pharmacodynamic modeling of ipamorelin, a growth hormone releasing peptide, in human volunteers. Pharm Res. 1999 Sep;16(9):1412-6. doi: 10.1023/a:1018955126402. PMID: 10496658. https://pubmed.ncbi.nlm.nih.gov/10496658/
- Schally AV, Zhang X, Cai R, Hare JM, Granata R, Bartoli M. Actions and Potential Therapeutic Applications of Growth Hormone-Releasing Hormone Agonists. Endocrinology. 2019 Jul 1;160(7):1600-1612. doi: 10.1210/en.2019-00111. PMID: 31070727. https://pubmed.ncbi.nlm.nih.gov/31070727/
- Schally AV, Zhang X, Cai R, Hare JM, Granata R, Bartoli M. Actions and Potential Therapeutic Applications of Growth Hormone-Releasing Hormone Agonists. Endocrinology. 2019 Jul 1;160(7):1600-1612. https://pubmed.ncbi.nlm.nih.gov/31070727/
- Sinha, D. K., Balasubramanian, A., Tatem, A. J., Rivera-Mirabal, J., Yu, J., Kovac, J., Pastuszak, A. W., & Lipshultz, L. I. (2020). Beyond the androgen receptor: the role of growth hormone secretagogues in the modern management of body composition in hypogonadal males. Translational andrology and urology, 9(Suppl 2), S149–S159. https://doi.org/10.21037/tau.2019.11.30
- Bill, C. A., & Vines, C. M. (2020). Phospholipase C. Advances in experimental medicine and biology, 1131, 215–242. https://doi.org/10.1007/978-3-030-12457-1_9
- Lall, S., Tung, L. Y., Ohlsson, C., Jansson, J. O., & Dickson, S. L. (2001). Growth hormone (GH)-independent stimulation of adiposity by GH secretagogues. Biochemical and biophysical research communications, 280(1), 132–138. https://doi.org/10.1006/bbrc.2000.4065
- Sabrina Lall, Loraine Y.C Tung, Claes Ohlsson, John-Olov Jansson, Suzanne L Dickson, Growth Hormone (GH)-Independent Stimulation of Adiposity by GH Secretagogues, Biochemical and Biophysical Research Communications, Volume 280, Issue 1, 2001, Pages 132-138, ISSN 0006-291X, https://doi.org/10.1006/bbrc.2000.4065
- Image 1 source: National Center for Biotechnology Information. PubChem Compound Summary for CID 91976842, CJC1295 Without DAC. https://pubchem.ncbi.nlm.nih.gov/compound/CJC1295-Without-DAC
- Image 2 source: National Center for Biotechnology Information (2024). PubChem Compound Summary for CID 9831659, Ipamorelin. https://pubchem.ncbi.nlm.nih.gov/compound/Ipamorelin.