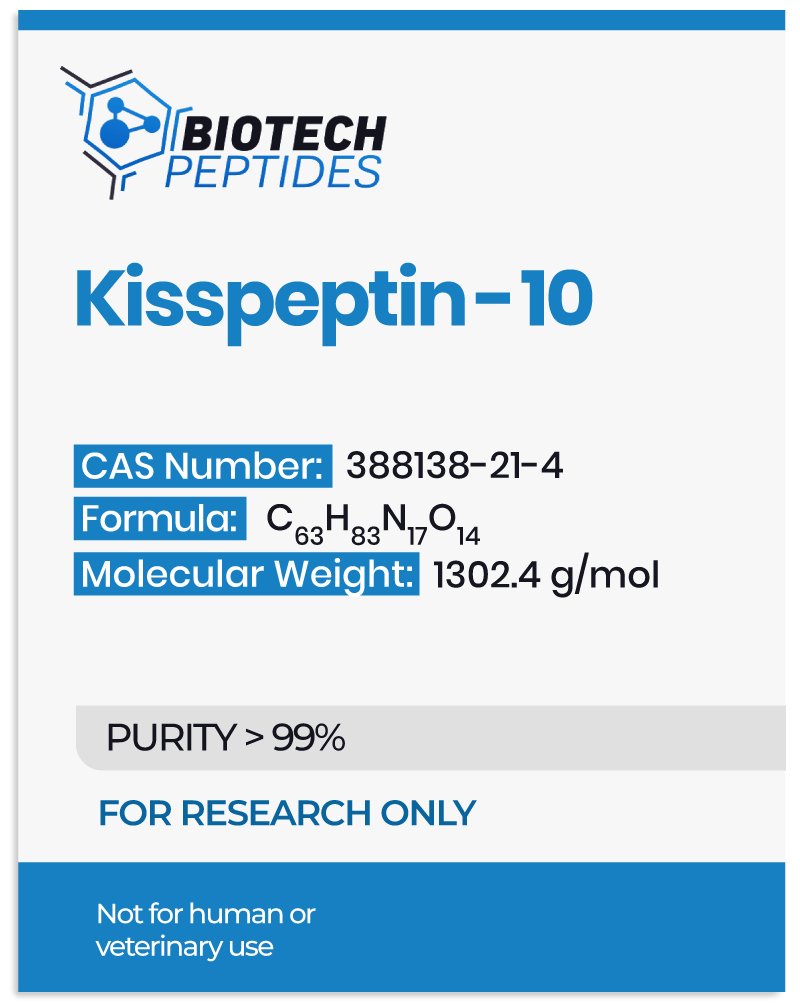
The Potential Function of Kisspeptin-10
Testosterone Secretion
Kisspeptin-10 peptide may affect and influence testosterone levels by modulating FSH and LH levels in the circulatory system, which is sex-specific. Kisspeptin-10 might increase testosterone levels in male species but has no perceived effect on testosterone levels in female species.
Kisspeptin-10 peptide analogs may influence the pulse frequency of LH in males, implying that Kisspeptin-10 might possibly fine-tune the regular pulsatile release of sex hormones.
Studies examining Kisspeptin-10 in male organisms suggest a concentration-dependent and rapid increase in serum LH and testosterone levels. Kisspeptin-10 may accomplish this by increasing the pulsatile release of LH. High concentrations of Kisspeptin-10 peptide may cause rapid pulsation, resulting in continuous LH release.
Gonadotropin-Releasing Hormone
GnRH neurons in the hypothalamus appear to synthesize and release gonadotropin-releasing hormone (GnRH). The first hypothalamic-pituitary-gonadal hormonal release may influence the anterior pituitary gland to release FSH and luteinizing hormone (LH). The primary hormone for reproductive development and the control of gamete maturation in the genitals is considered to be GnRH.
Kisspeptin-10 Peptide and Energy
Kisspeptin-10 peptide neurons may be energy status sensitive: undernutrition and overnutrition may inhibit Kisspeptin-10 neurons’ ability to induce GnRH release.[3] Infertility may occur in males and females alike under extreme energy balance conditions, mediated by the Kisspeptin-10 peptide. As a result, Kisspeptin-10 peptide synthesis and release may be energy balance sensitive. However, the findings suggest that Kisspeptin-10 may be the sole regulator of energy balance.
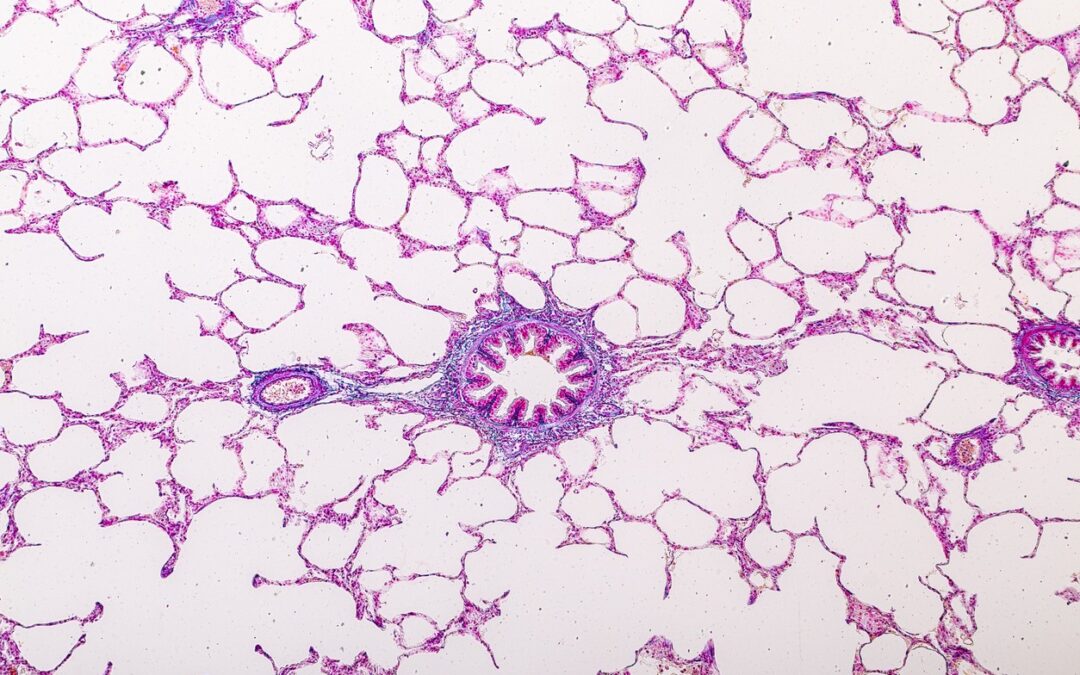
Studies in mice samples depleted of the Kisspeptin-10 receptor (Kiss1r) via genetic manipulation suggest an increase in adiposity and a decrease in energy expenditure. Studies suggest that Kisspeptin-10 receptors exist in adipose (fat) and brown adipose tissues. Kisspeptin-10 peptide may also help to explain the neurochemical modulation that results in energy-modulating behavior concerning reproduction.
Kisspeptin-10 Peptide and Mood
A study examining Kisspeptin suggested that the peptide may have increased limbic brain activity.[4] There was a reported increase in drive, reward-seeking behavior, and overall improved mood. Kisspeptin-10 peptide appeared to accomplish this by integrating the emotional brain and the sexual process through the overall reproduction process.
Kisspeptin-10 Peptide and the Heart
Kisspeptin-10 peptide and its receptors are considered to be found in numerous locations throughout the kidney and may play an essential role in stimulating kidney functions, according to the findings. Animal studies in mice lacking the Kiss1 receptor suggest that the peptide may be critical for maintaining glomerular development during development, though whether this action is direct or indirect is unknown.
Although the function of Kisspeptin-10 peptide in the kidney is unknown, the peptide may influence vascular development and injury responses. Kisspeptin-10 studies in mice with cardiovascular disease suggest that the peptide may act in the vascular beds, controlling vasoconstriction.
The potential of Kisspeptin-10 peptide on angiogenesis and vascular function may significantly impact the kidney and cardiovascular system.
Kisspeptin-10 Peptide and Memory
Research studies in mice suggest that Kisspeptin analogs may reverse the navigational and learning impairment caused by ethanol intoxication. Kisspeptin-10 peptide and its analogs may potentially play a role in neurons encoding information and compensating for learning defects in certain genetic and chronic disease conditions.
Kisspeptin-10 Peptide and Cancer
Kisspeptin-10 peptide was discovered about 20 years ago and suggested to suppress melanoma metastasis by approximately 95%, indicating that the peptide may have an effect to reduce cancer cell spread. The evaluation of various metastatic cancers suggests that Kisspeptin-10 levels may decrease in the bladder, GI, breast, pancreatic, ovarian, thyroid, skin, and prostate, suggesting that the peptide may exert some role in cancer spread.
In 2020, an experiment on Kisspeptin-10 peptide levels under daylight exposure established a potential link between melatonin, kisspeptin-10, and cancer.[5] Findings in mice models exposed to daylight supported findings of high levels of Kisspeptin and low melatonin levels, and vice versa in the dark. In daylight mice, there was no appearance of increase in tumor growth rates, metastasis, or volume. Kisspeptin-10 and melatonin may be implicated in tumor suppression as one appears to influence the actions of the other, though the precise relationship is unknown.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References
- Jayasena CN, Nijher GM, Comninos AN, Abbara A, Januszewki A, Vaal ML, Sriskandarajah L, Murphy KG, Farzad Z, Ghatei MA, Bloom SR, Dhillo WS. The effects of kisspeptin-10 on reproductive hormone release show sexual dimorphism in humans. J Clin Endocrinol Metab. 2011 Dec;96(12):E1963-72. doi: 10.1210/jc.2011-1408. Epub 2011 Oct 5. PMID: 21976724; PMCID: PMC3232613.
- George JT, Veldhuis JD, Roseweir AK, Newton CL, Faccenda E, Millar RP, Anderson RA. Kisspeptin-10 is a potent stimulator of LH and increases pulse frequency in men. J Clin Endocrinol Metab. 2011 Aug;96(8):E1228-36. doi: 10.1210/jc.2011-0089. Epub 2011 Jun 1. PMID: 21632807; PMCID: PMC3380939.
- Navarro VM. Metabolic regulation of kisspeptin – the link between energy balance and reproduction. Nat Rev Endocrinol. 2020 Aug;16(8):407-420. doi: 10.1038/s41574-020-0363-7. Epub 2020 May 19. PMID: 32427949; PMCID: PMC8852368.
- Comninos AN, Wall MB, Demetriou L, Shah AJ, Clarke SA, Narayanaswamy S, Nesbitt A, Izzi-Engbeaya C, Prague JK, Abbara A, Ratnasabapathy R, Salem V, Nijher GM, Jayasena CN, Tanner M, Bassett P, Mehta A, Rabiner EA, Hönigsperger C, Silva MR, Brandtzaeg OK, Lundanes E, Wilson SR, Brown RC, Thomas SA, Bloom SR, Dhillo WS. Kisspeptin modulates sexual and emotional brain processing in humans. J Clin Invest. 2017 Feb 1;127(2):709-719. doi: 10.1172/JCI89519. Epub 2017 Jan 23. PMID: 28112678; PMCID: PMC5272173.
- Pazarci P, Kaplan H, Alptekin D, Yilmaz M, Lüleyap U, Singirik E, Pelit A, Kasap H, Yegani A. The effects of daylight exposure on melatonin levels, Kiss1 expression, and melanoma formation in mice. Croat Med J. 2020 Feb 29;61(1):55-61. doi: 10.3325/cmj.2020.61.55. PMID: 32118379; PMCID: PMC7063558.