Copper Peptide (AHK-Cu) and Hair Follicle Regeneration
What is AHK-Cu Peptide?
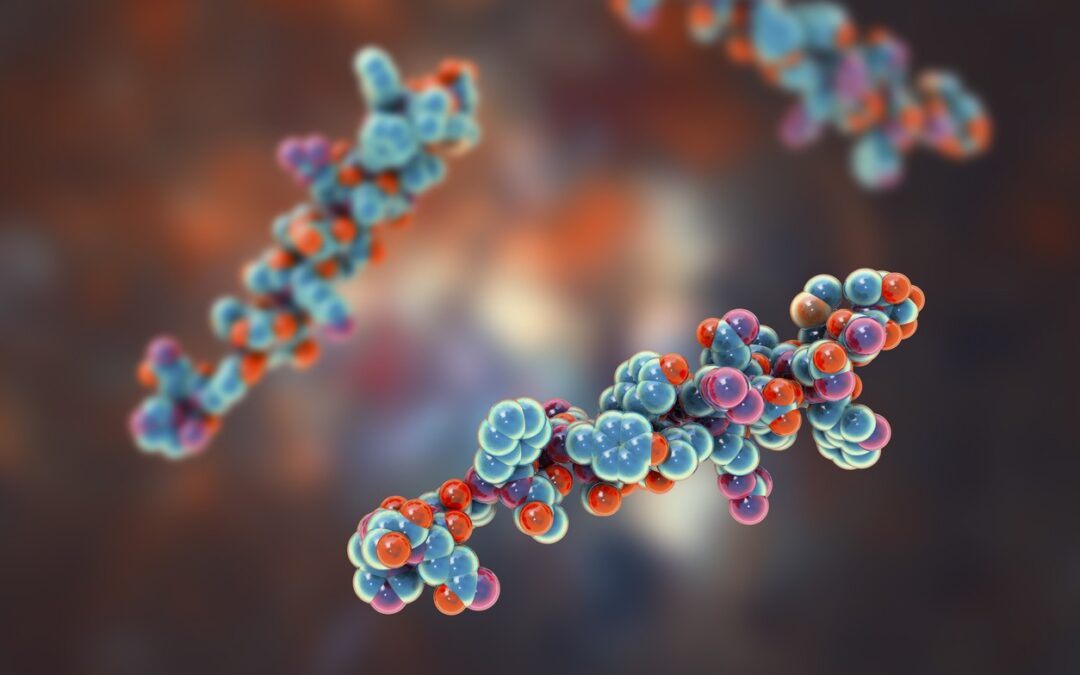
AHK-Cu is a short peptide with three amino acids attached to a copper molecule (Ala-His-Lys-Cu). AHK-Cu peptide, also known as copper peptide, has been isolated in blood samples. This peptide may be responsible, in part, for growth and development of cells in the blood vessels. It has also been researched in relation to the generation of new blood vessels (angiogenesis). These actions of the AHK-Cu peptide are posited to be due to its potential to stimulate the production of another peptide called the Vascular Endothelial Growth Factor (VEGF). Producing new blood cells may help supply blood to biological structures such as skin and hair follicles, and may stimulate their development.
Researchers have also studied AHK-Cu in relation to its potential impact on Growth Factor Beta-1. Through its potential impact on Growth Factor Beta-1 and VEGF, AHK-Cu peptide may activate the replication and development of fibroblast cells. Fibroblasts are cells abundantly found in biological structures, including skin, hair follicles, and blood vessels. Fibroblasts are considered to activate the production of proteins such as elastin and collagen, essential participants of the extracellular matrix in the skin.
Research on AHK-Cu Peptide
Follicle Growth and Maintenance
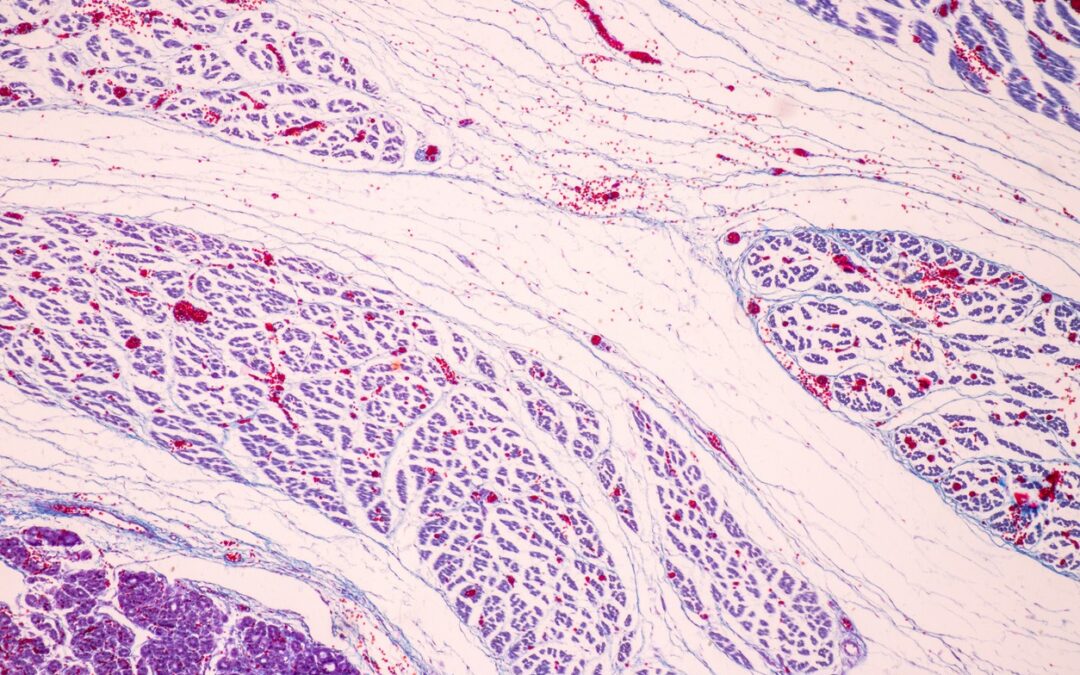
AHK-Cu peptide may potentiate immense growth on follicle development and maintenance. Researchers suggest it may supplement follicle density by preventing possible loss and by stimulating new growth. Follicles may be found in highly vascular structures, areas where extensive network of blood vessels are concentrated, to supply blood to developing follicles. The supply of blood is considered to be crucial because follicles undergo a rapid cell turnover and appear to depend on the supply of blood and nutrients in the process. Along those same lines, blood supply has been suggested to limit the production of, and stability of existing follicles. AHK-Cu peptide may potentially promote new blood vessel development by triggering the release of VEGF.
Another important phenomenon that may potentially damage follicle development is the excessive conversion of testosterone to dihydrotestosterone (DHT). Researchers consider it to be a potentially critical pathology in certain conditions characterized by immense hair loss. AHK-Cu peptide might be relevant in these contexts, as researchers suggest it may prevent the conversion of testosterone to DHT. Second, it may potentially down-regulate the action of DHT on hair follicle receptors.
The hair follicles appear to undergo three main phases of growth: anagen, catagen, and telogen phase. The anagen phase is the growth phase of follicles, and is a highly active phase. Research suggests that AHK-Cu peptide may ‘trap’ the follicles in the anagen phase of the growth cycle and maintain that phase for a considerable duration (certain research findings suggest upwards of a year).
Cell Aging and Skin Structure
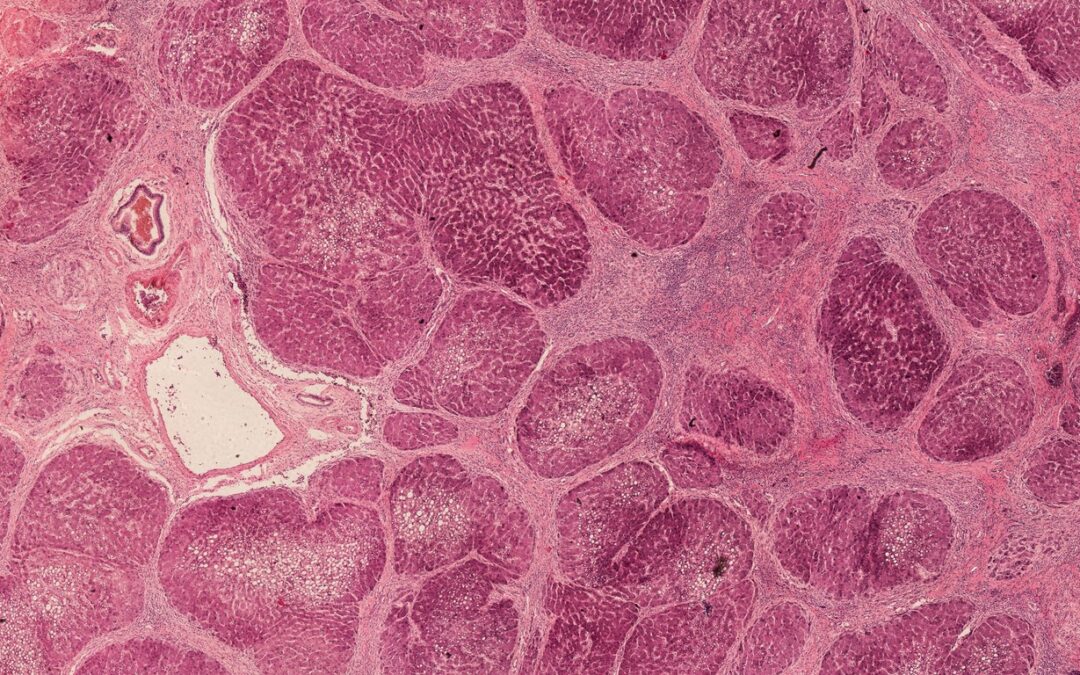
A subset of skin cells, fibroblasts are deemed responsible for the secretion of skin proteins such as collagen and elastin. These proteins are considered to lend the skin structure flexibility, and suppleness. Cell aging in the skin may lead to rapid decline in the number of fibroblasts. As a result, the amount of collagen and elastin endogenously produced begins to decline as well, introducing irregularities and textural inconsistencies in the skin and developing creases along the skin surface.
AHK-Cu peptide may potentiate the reversal of cell aging by triggering the growth and development of new fibroblasts. Once there are enough fibroblasts in the extracellular matrix of the skin, natural elastin and collagen production may follow. Research suggests that AHK-Cu may potentially stimulate the production of Type 1 collagen by up to 300%.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.